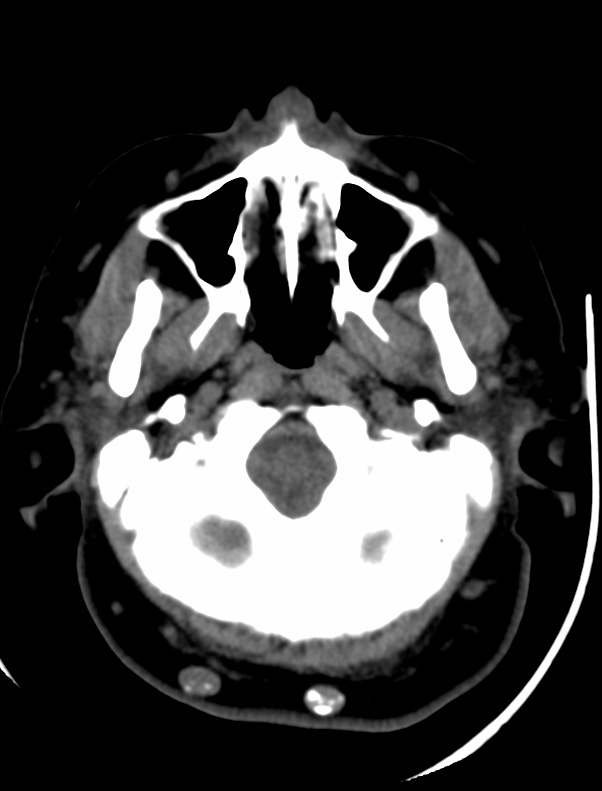

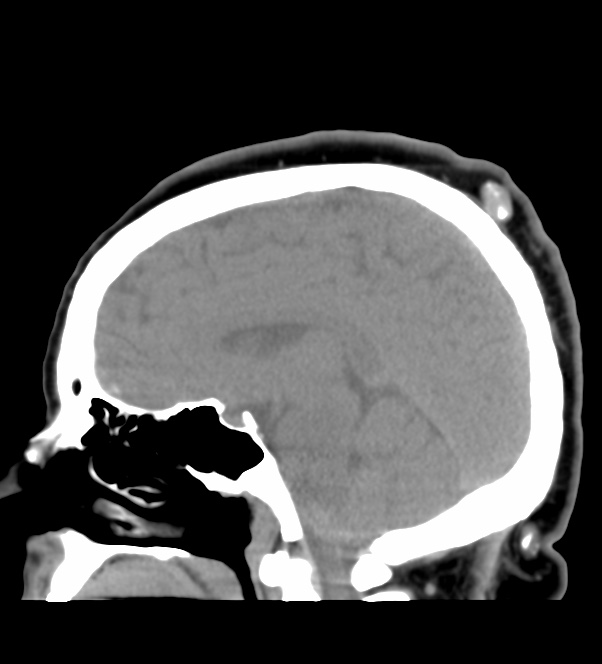
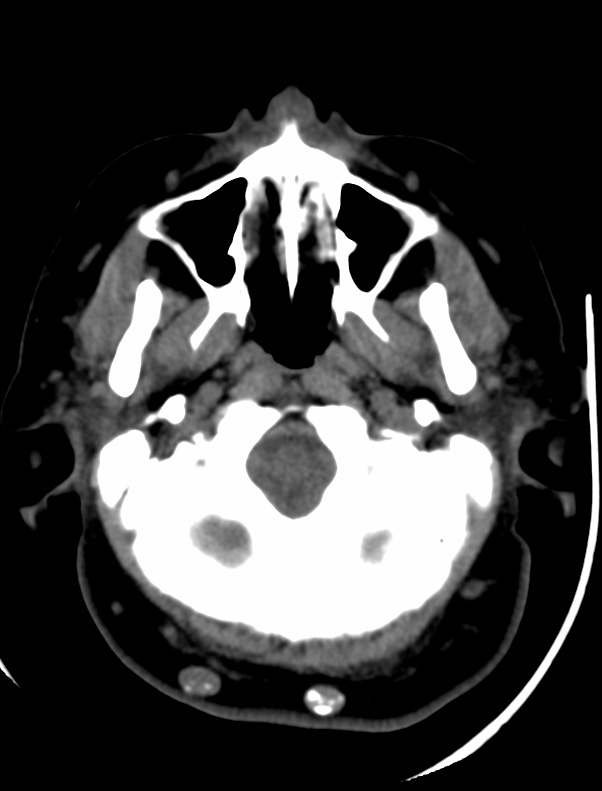
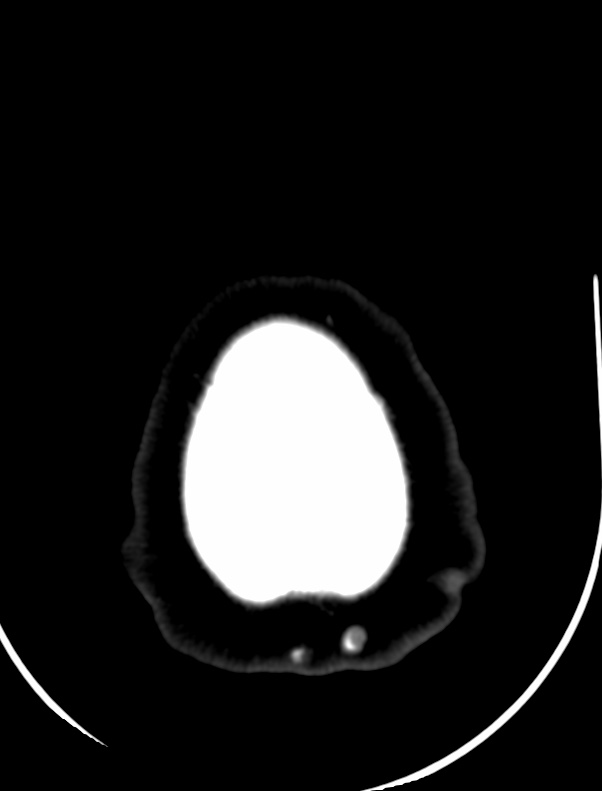
The usual clinical presentation of PTT is that of a long-standing, subcutaneous, cystic nodule that slowly progresses to a large, nodular mass, often following a history of trauma or inflammation. The tumor preferentially arises in areas of dense hair follicle concentrations, and about 90% of cases occur on the scalp, with the residual 10% occurring mainly on the back. Other, less common locations include the vulva, nose, mons pubis, buttock, wrist, chest, and elbow.
Women are affected in more than 80% of cases, and the average age of patients is 65 years . The presentation is nearly always that of a single lesion, but, rarely, multiple lesions are seen.
Areas of necrosis, calcification, and hyalinization may be seen. The stroma is usually fibrous and shows a variable inflammatory reaction, including foreign body giant cells.



Although PTT is generally considered biologically benign, even though histologically indistinguishable from squamous cell carcinoma in some cases, malignant PTT has been reported. Saida et al suggested three stages in the oncologic development of a malignant PTT: the adenomatous stage of the trichilemmal cyst, the epitheliomatous stage of the PTT, and the carcinomatous stage of the malignant PTT. A rare occurrence of PTT with spindle cell carcinoma has also been reported .
Reference:
American Journal of Neuroradiology January 2001, 22 (1) 180-183;