
Allergic fungal sinusitis is the most common form of fungal sinusitis. It is particularly common in warm, humid climates. The overall prevalence of allergic fungal sinusitis is estimated at 5%–10% of all patients with chronic hypertrophic sinus disease going to surgery.
The underlying cause is thought to be a hypersensitivity reaction to certain inhaled fungal organisms resulting in a chronic noninfectious, inflammatory process, similar to that seen in allergic bronchopulmonary aspergillosis of the lung. Although the exact pathophysiology is not yet clear, immunologically, immunoglobulin E–mediated type I immediate hypersensitivity and type III delayed hypersensitivity are thought to be involved.
Common implicated fungi are the dematiaceous (pigmented) fungi—Bipolaris, Curvularia, Alternaria—and the hyaline molds such as Aspergillus and Fusarium. Allergic fungal sinusitis is characterized by the presence within the affected sinuses of “allergic mucin”—inspissated mucus that is yellow-green, white-tan, gray, brown, or black with the consistency of peanut butter.


Allergic fungal sinusitis tends to be a disease of younger individuals, usually in their third decade. Typically, afflicted individuals are immunocompetent. There is a frequent associated history of atopy including allergic rhinitis and asthma. Patients usually experience chronic headaches, nasal congestion, and chronic sinusitis for several years. There is often a history of sinus surgery.
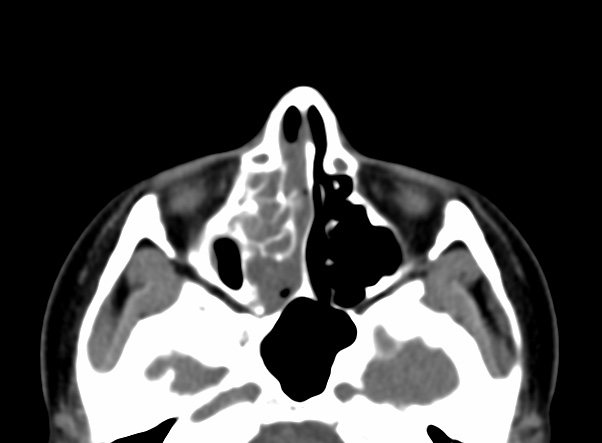
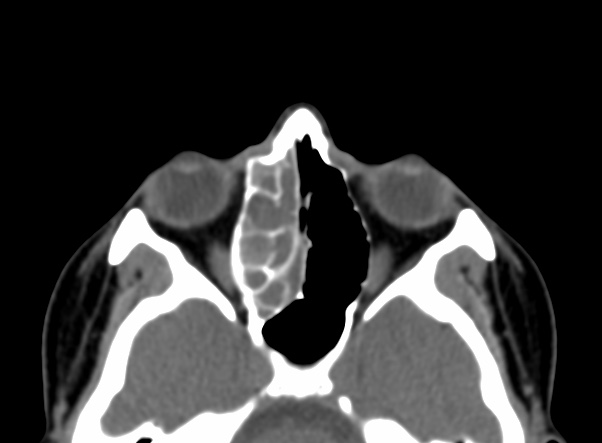
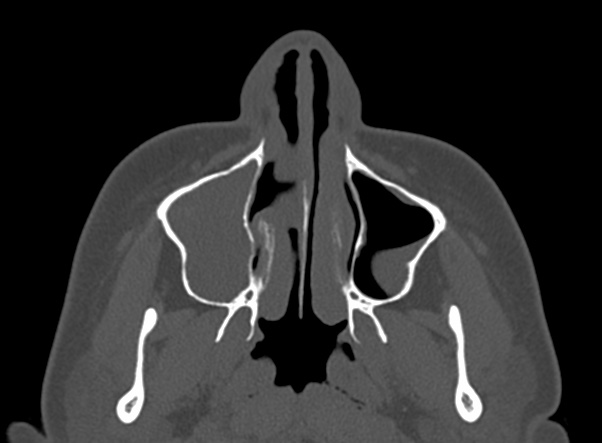
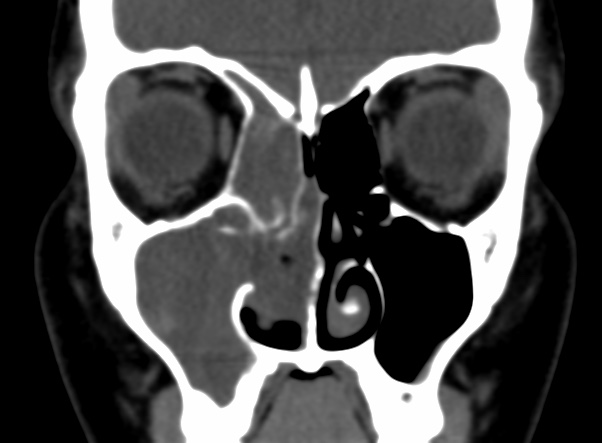
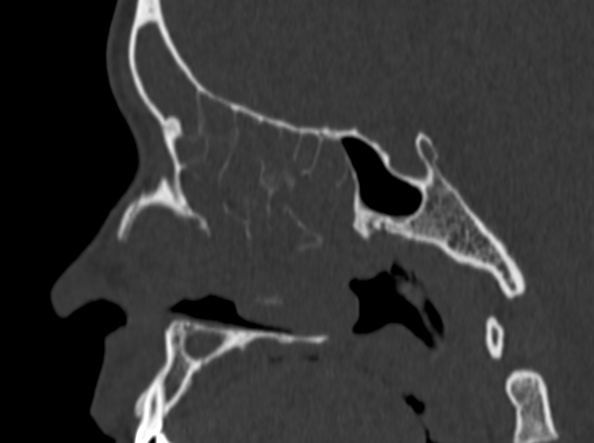
There is usually involvement of multiple sinuses if not pansinusitis and rhinitis. Disease tends to be bilateral, and there is a frequent nasal component. The majority of the sinuses show near-complete opacification and are expanded. Expansion, remodeling, or thinning of involved sinus walls is common in allergic fungal sinusitis (AFS) and is thought to be caused by the expansile nature of the accumulating mucin. Areas of high attenuation are found within the expanded paranasal sinuses in all patients. Similar radiographic findings can be caused by rare osteoid/chondroid matrix-producing sinonasal sarcomas or meningiomas.
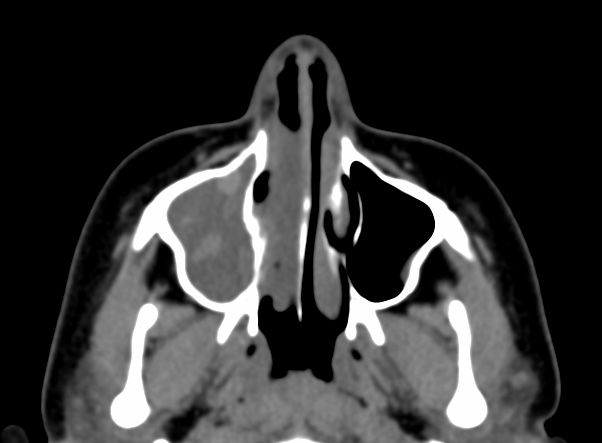
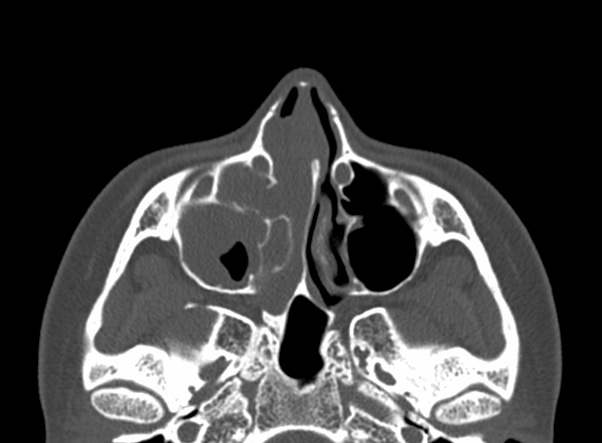
Noncontrast CT demonstrates hyperattenuating allergic mucin within the lumen of the paranasal sinus.





Bony erosion of the sinus walls and extension into adjacent cavities have been mentioned in many reports, usually focusing on intracranial extension, as depicted in the 1st image above. In most series, a rate of approximately 20% bony erosion with extension into surrounding vital cavities is reported.
The ethmoid sinus was the most commonly involved sinus, while the adjacent lamina papyracea was the most common bone to exhibit demineralization, as depicted in the image below. Extension of allergic fungal sinusitis (AFS) beyond the confines of the paranasal sinuses most commonly occurred into the orbit, followed by the anterior, middle, and posterior cranial fossae, respectively
Although low signal intensity of the sinus contents has been described on T1-weighted images, we have frequently observed high signal intensity or mixed low, intermediate, and high signal intensity on T1-weighted images in these patients. There is characteristic low signal intensity or signal void on T2-weighted images. The T2 signal void is attributed to a high concentration of various metals such as iron, magnesium, and manganese concentrated by the fungal organisms. The T2 signal void is also attributed to a high protein and low free-water content of the allergic mucin.
The inflamed mucosal lining is relatively hypointense on T1-weighted images and hyperintense on T2-weighted images and demonstrates enhancement after intravenous administration of gadolinium contrast material.
There is no enhancement in the center or in majority of the sinus contents, which distinguishes this condition from neoplastic entities.
Although the condition is not considered invasive, if left untreated, the involved sinuses expand and there is smooth bone erosion with subsequent intracranial or intraorbital extension and resulting cranial or orbital symptoms. Intracranial extension is usually limited by the dura to the extradural space.
Reference: