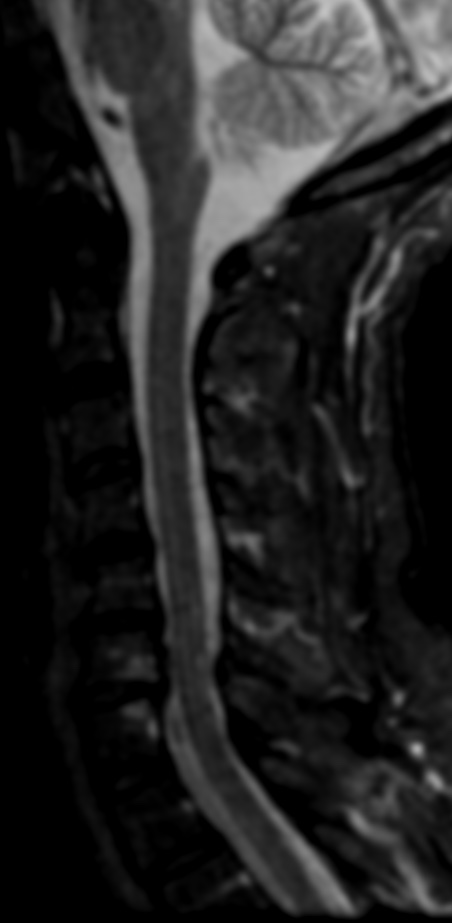


Posterior cervical myelopathy refers to a condition where there is compression of the spinal cord in the cervical spine, specifically in the posterior region of the spine. MRI is a useful imaging modality for evaluating cervical myelopathy, as it can show the extent and location of spinal cord compression.
On MRI, findings of posterior cervical myelopathy may include:
- Narrowing of the spinal canal: The spinal canal may appear narrower than normal due to degenerative changes, herniated discs, or bone spurs. This narrowing can lead to compression of the spinal cord.
- Signal changes in the spinal cord: Compression of the spinal cord can cause changes in the signal intensity of the spinal cord on MRI. These changes may be due to edema, myelomalacia, or gliosis .
- Disc herniation: Herniated discs can compress the spinal cord and lead to symptoms of myelopathy. On MRI, a herniated disc can be visualized as a bulging or protruding disc material beyond the normal confines of the disc space.
- Osteophytes or bone spurs: Osteophytes or bone spurs may form along the edges of vertebral bodies due to degenerative changes. These spurs can impinge on the spinal cord and cause compression.
- Ligamentum flavum hypertrophy: The ligamentum flavum is a ligament that runs along the back of the spinal canal. It can become thickened or hypertrophied due to degenerative changes, which can lead to compression of the spinal cord.