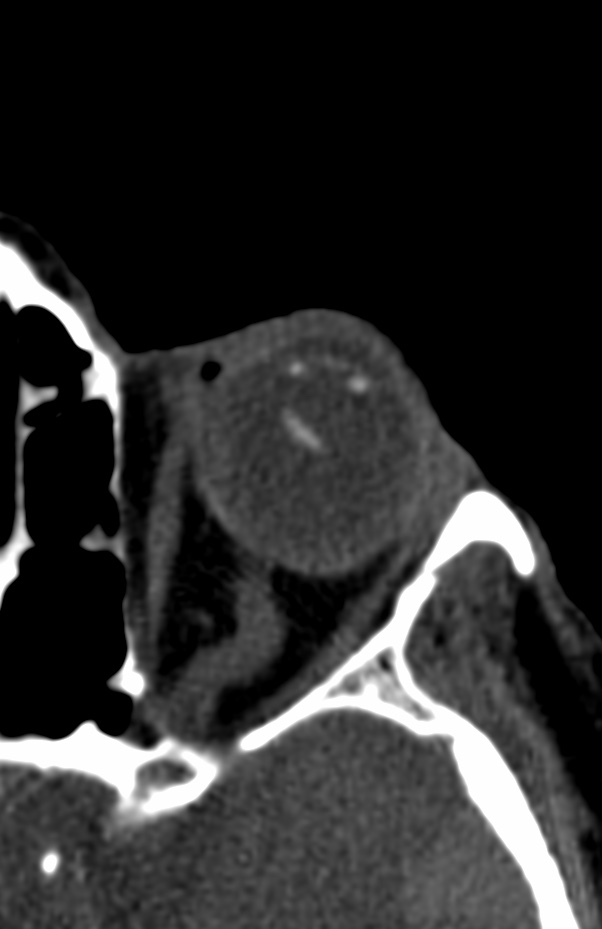
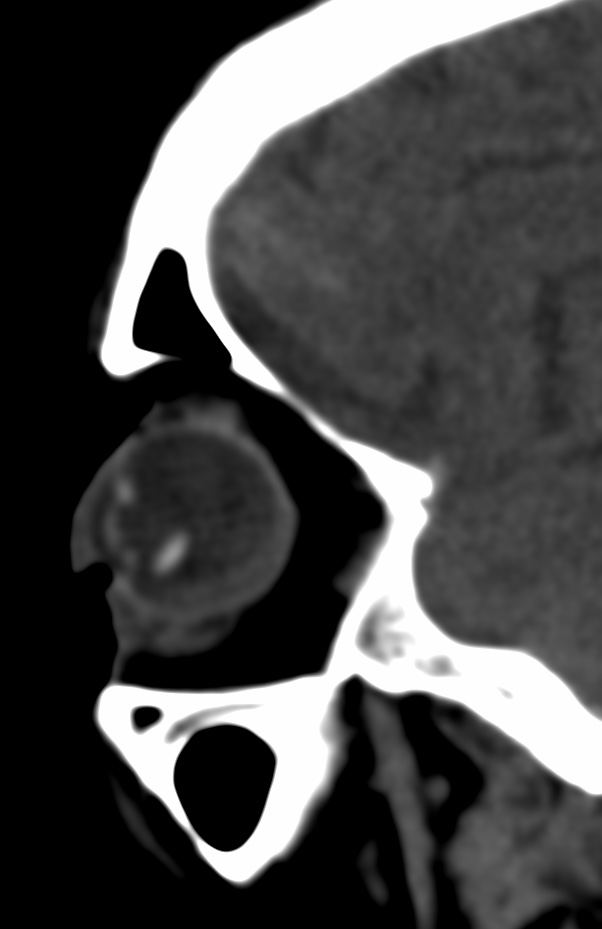
Blunt trauma may cause sudden compressive deformation of the globe causing transient shortening of the eye in the anterior-posterior direction displacing the cornea and anterior sclera posteriorly. This causes a compensatory expansion of the globe in the equatorial plane, which can stretch or break the zonules.
Partial or complete disruption of zonular fibers leads to subluxation or dislocation of the lens into the posterior chamber.
The differentiation between complete and partial zonular tear is essential as it can alter management.
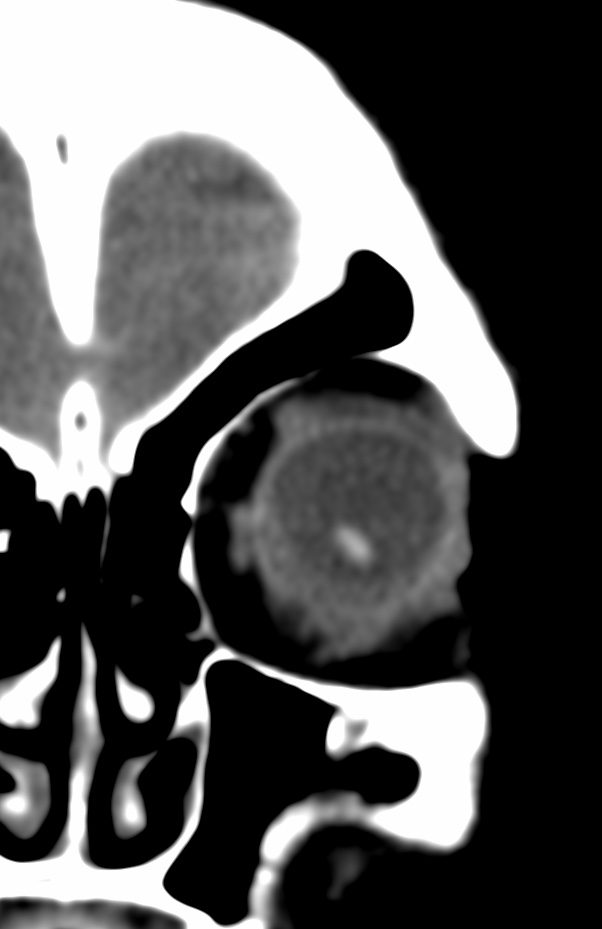
Radiologic imaging is not a substitute for a thorough direct ophthalmologic examination, it may be of occasional help in cases where a direct examination is not immediately possible which may be the case in a noncooperative patient (inebriated or posttraumatic) or due to extensive soft tissue injury. Thus, knowledge of this condition is essential and meticulous evaluation of the orbit and its contents is imperative in all routine CT scan of the heads, not only for medicolegal documentation purposes but also for prompt recognition and intervention.



Beside trauma, lens dislocation is seen in hereditary disorder like congenital aniridia, congenital glaucoma, cystathionine b-synthase deficiency, Ehlers-Danlos syndrome, focal dermal hypoplasia, homocystinuria, Kniest dysplasia, Marfan’s syndrome, molybdenum cofactor deficiency, sulfite oxidase deficiency, Weill-Marchesani syndrome.
Direction of dislocation dictates management. Anterior lens dislocation requires lens removal. Refractory glaucoma, persistent uveitis, or corneal damage are indications for urgent or emergent intervention. Posterior dislocation may be managed conservatively by correction with aphakic contact lenses. Lens removal in posterior dislocations should be considered in patients that do not tolerate correction, suffer symptoms despite correction, or develop glaucoma or persistent uveitis. If the patient undergoes surgery for another posterior chamber pathology lens removal may also be considered.
Reference: