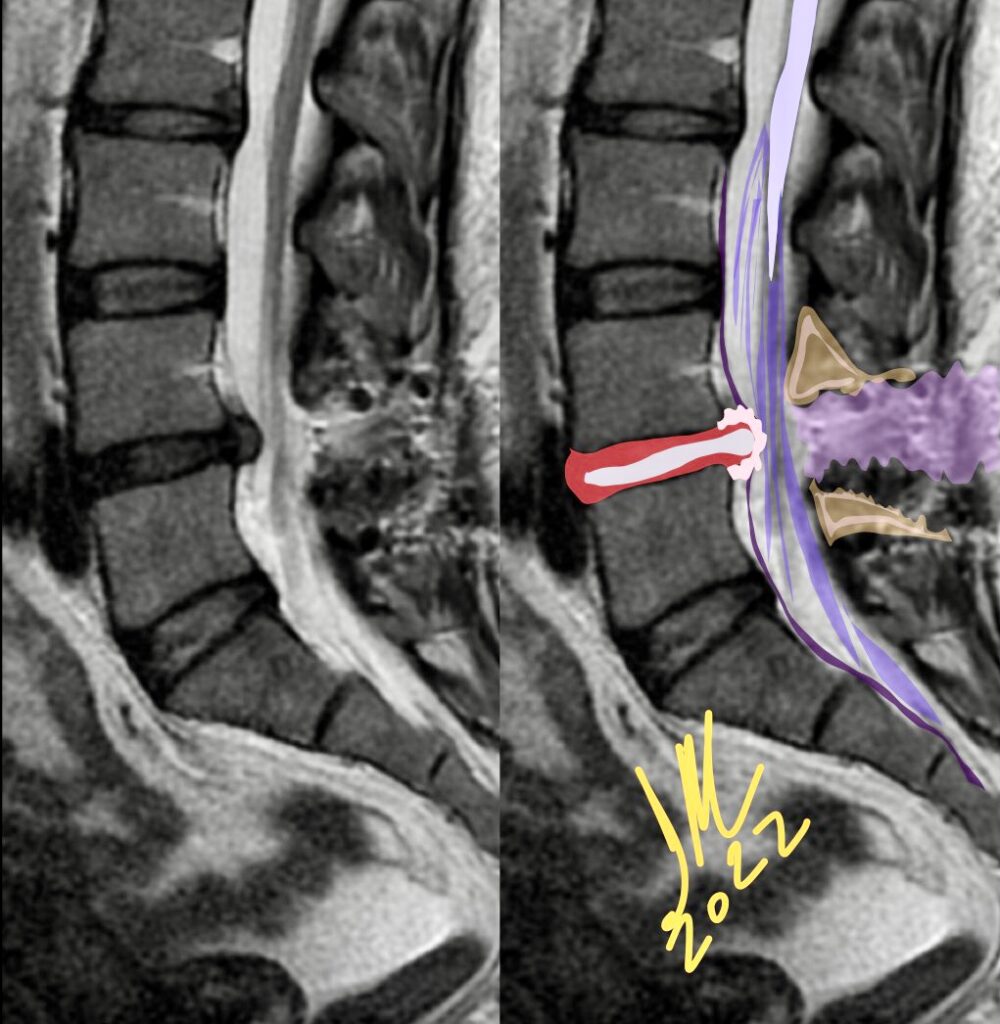
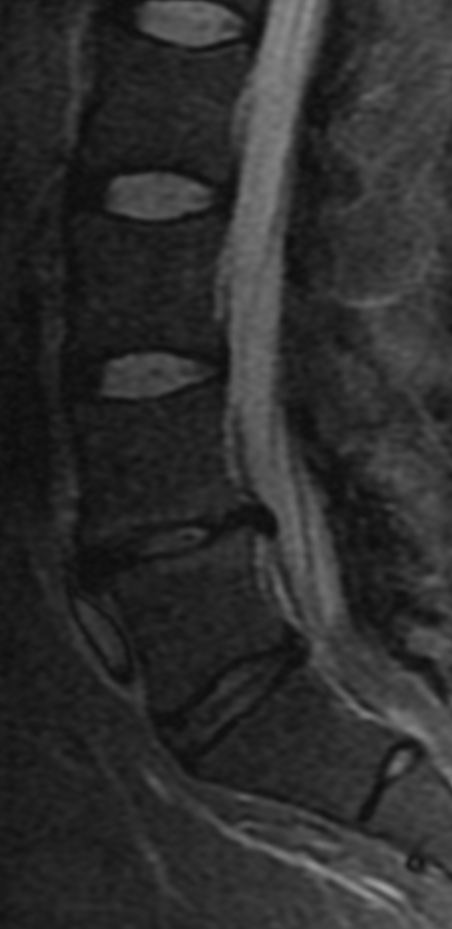
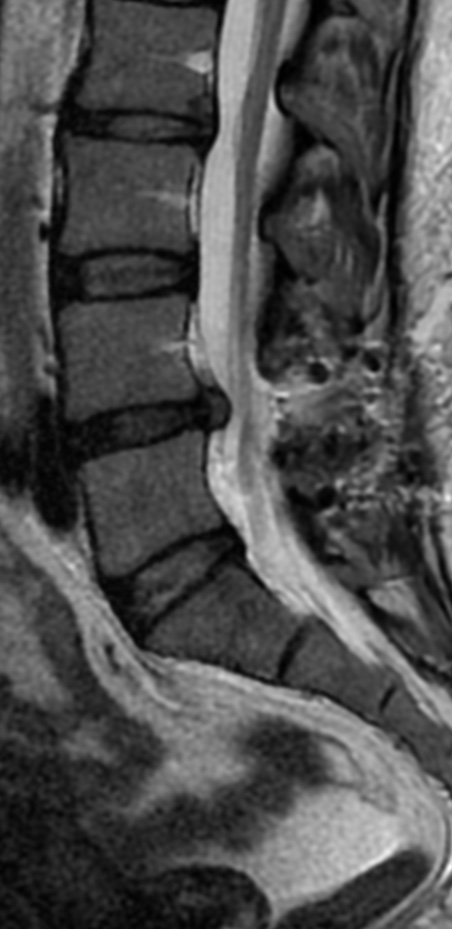
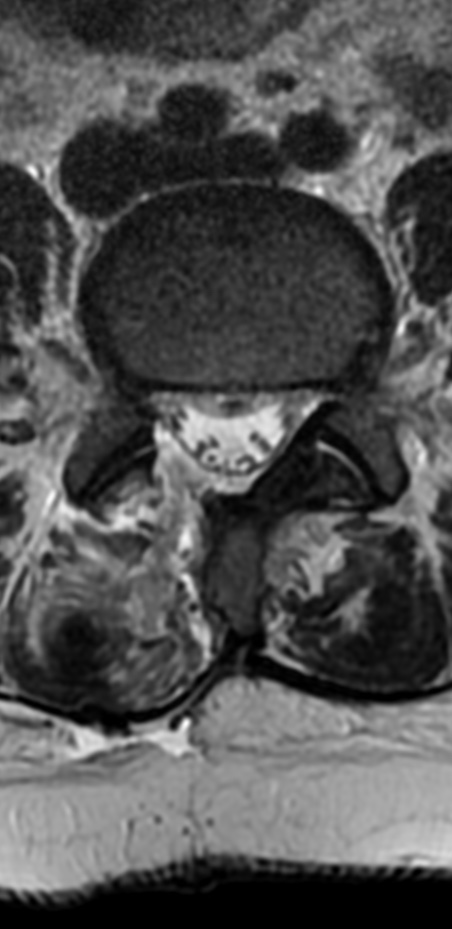
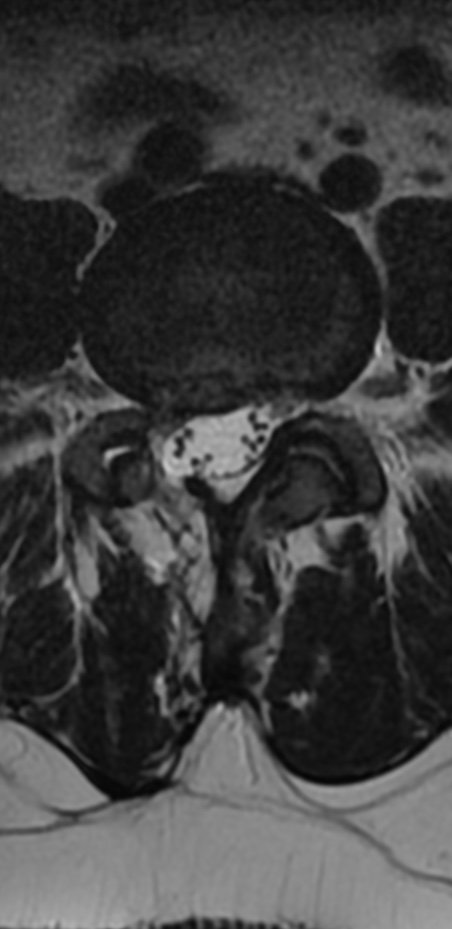
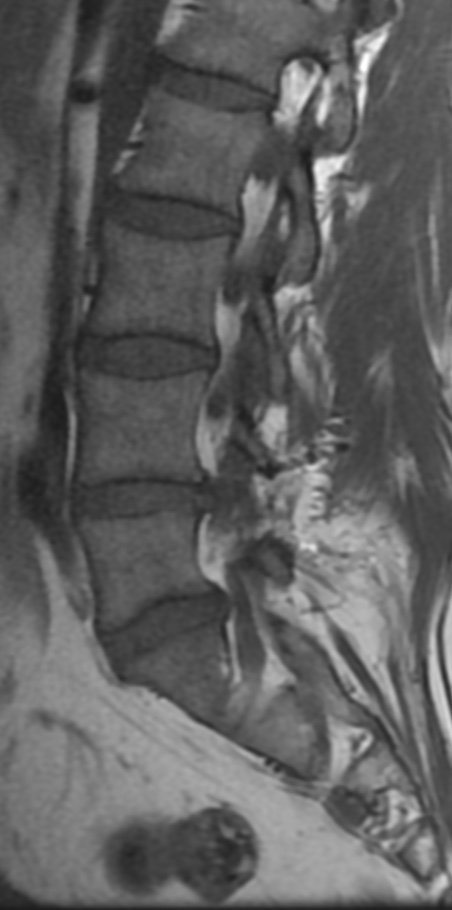
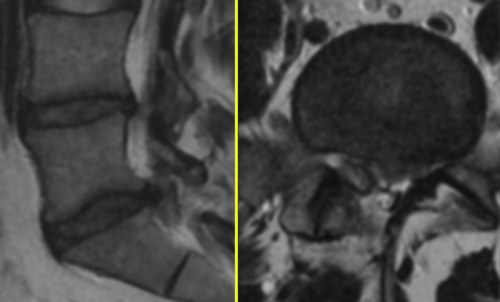
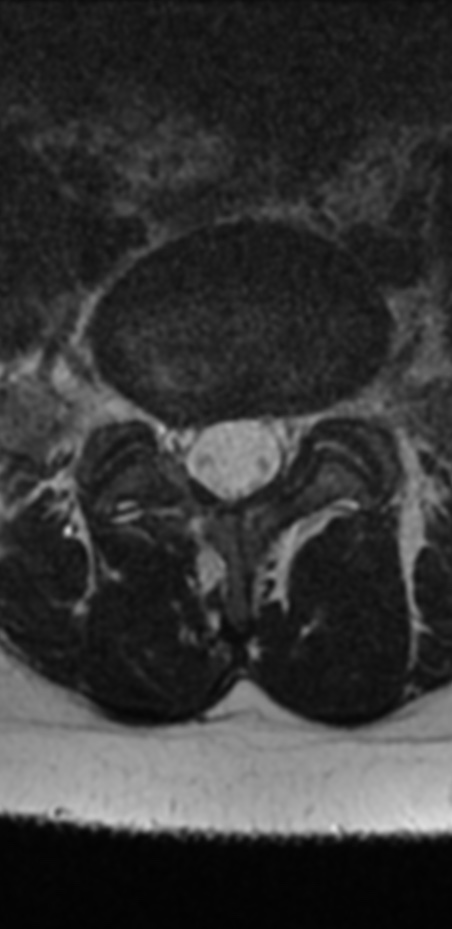
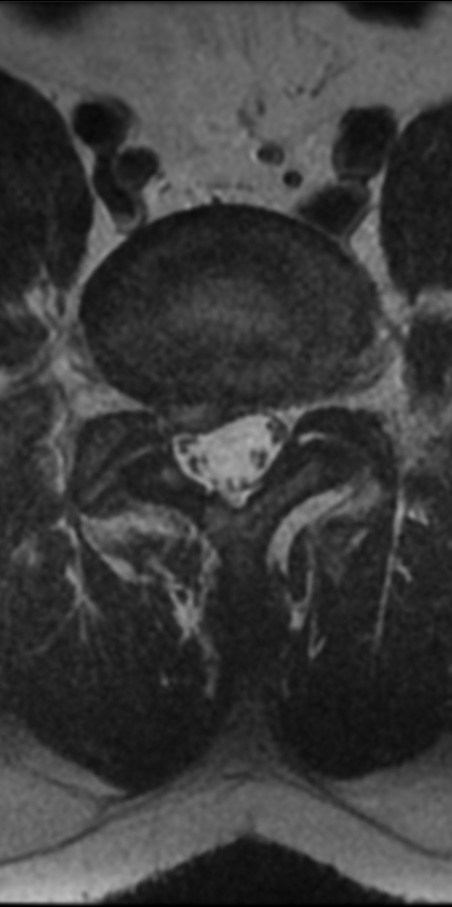
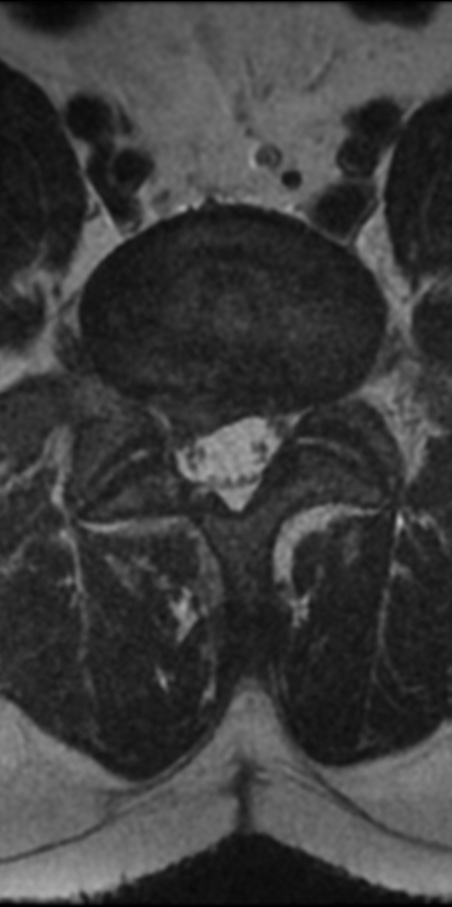
Recurrent lumbar disc herniation is defined as disc herniation at a previously operated disc level, regardless of ipsilateral or contralateral herniation, in patients who experienced a pain-free interval of at least 6 months after surgery.
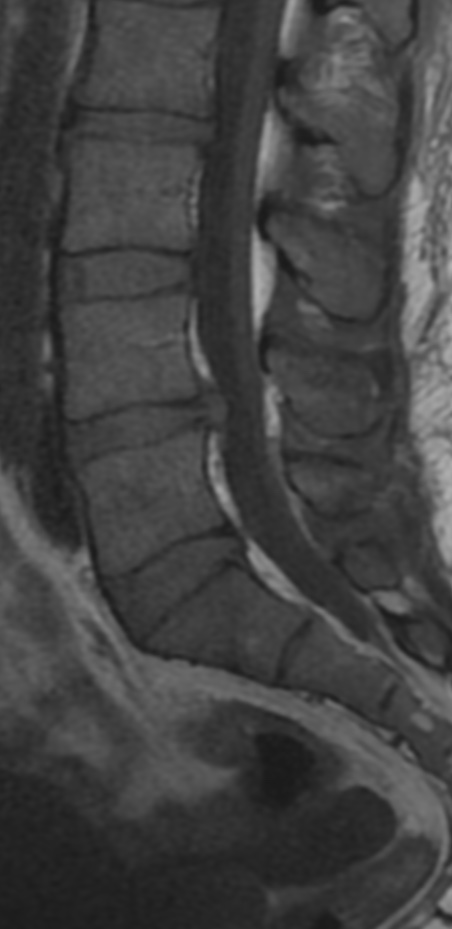
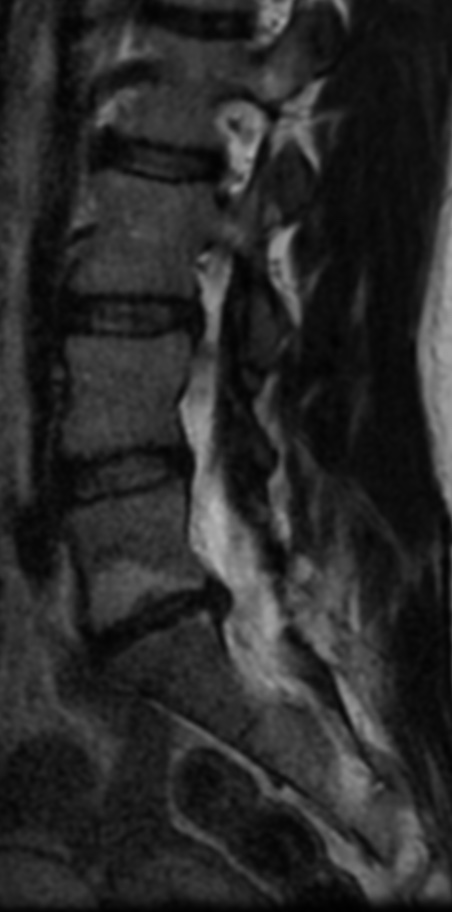
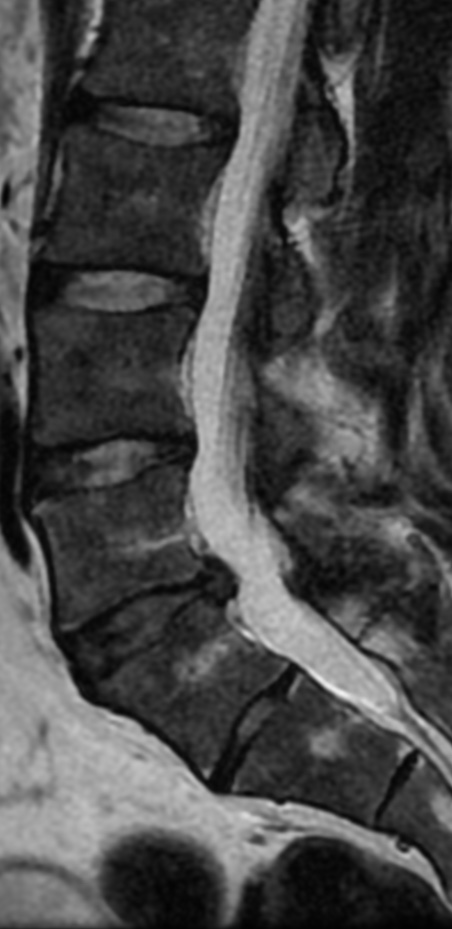
The highest revision rate 42% occurred at level L4–L5, followed by level L5–S1 in 25.0%.
There is significant association between disc degeneration assessed with the Pfirrmann disc degeneration grade and recurrent herniated lumbar disc (HLD) revision.
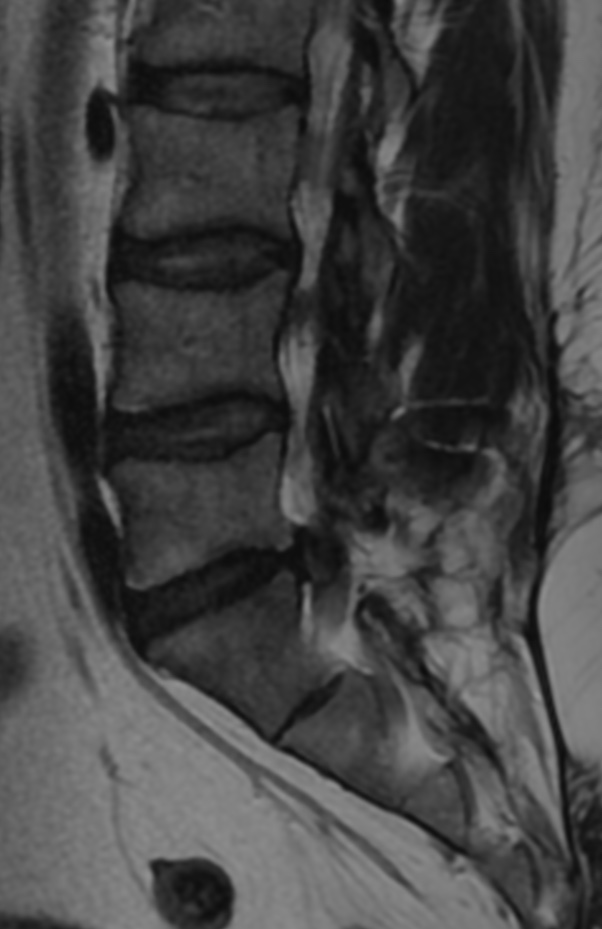
Cinotti et al. reported that, in severe degenerative disc patients, the annulus fibrosus showed a markedly low recovery rate after primary lumbar discectomy (LD), and the attenuated portion of the annulus fibrosus would aggravate recurrent HLD.
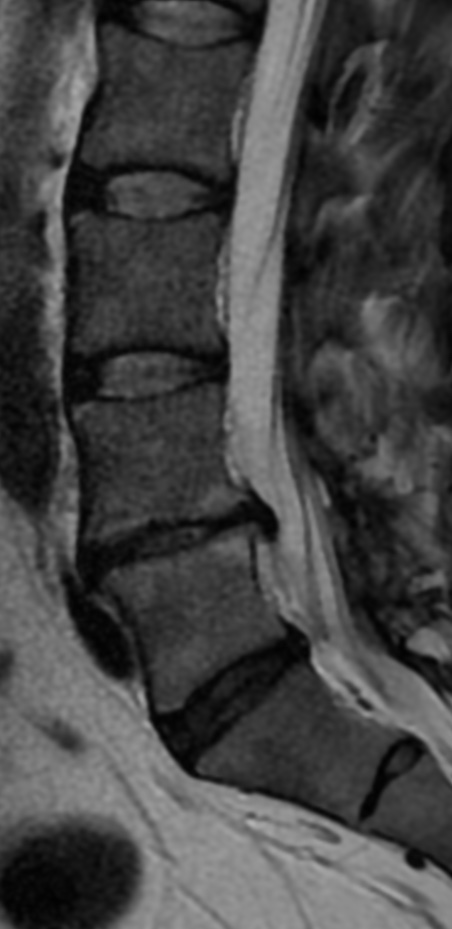
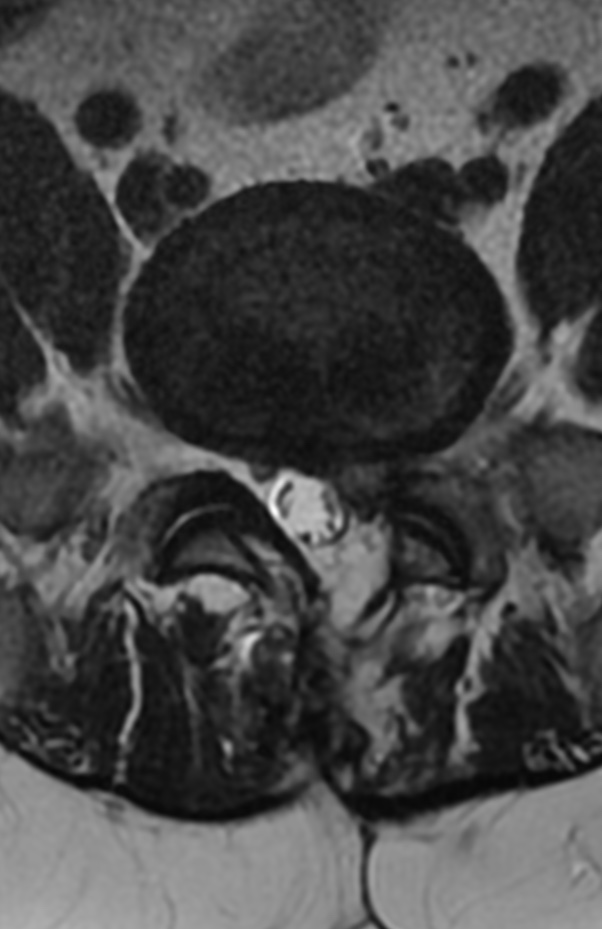
However, Dora et al. reviewed the relationship between disc degeneration assessed with five grading systems and HLD recurrence. They reported that patients with relatively low-grade disc degeneration had a greater risk of recurrence. However, they included 60 non-randomized patients into each of the study and control groups. The correlation between age and Pfirrmann grade was found to be significant by Okada et al.
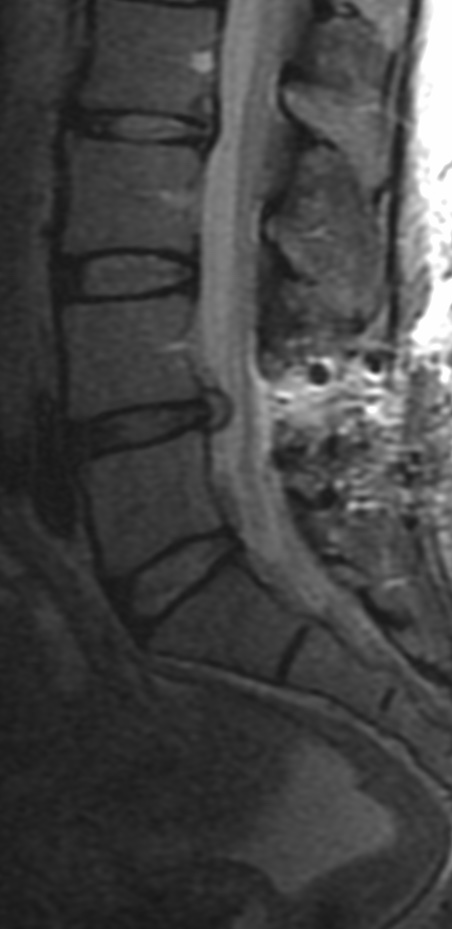
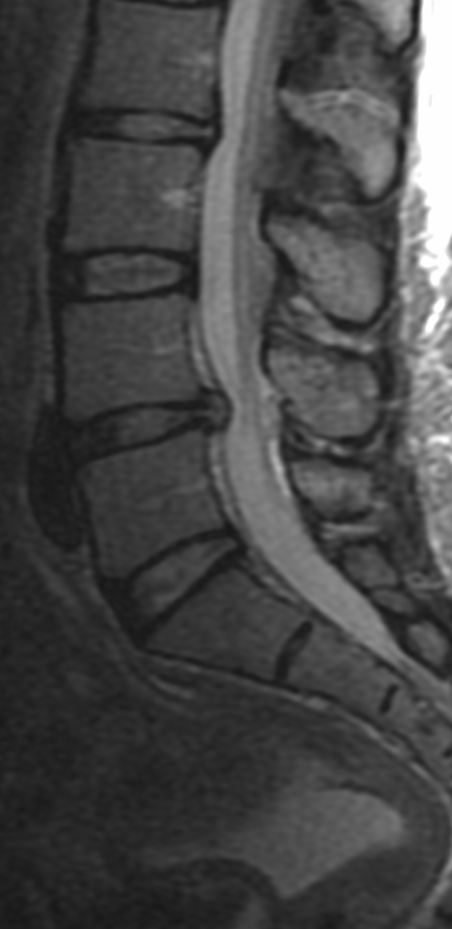

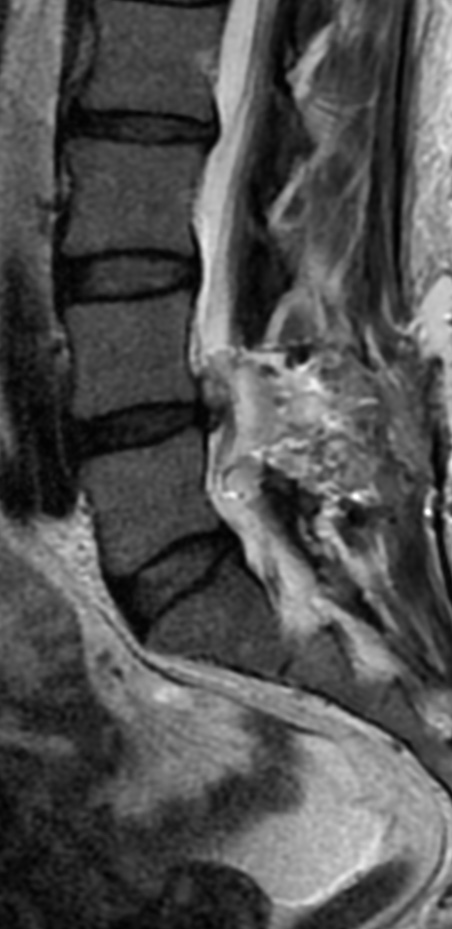
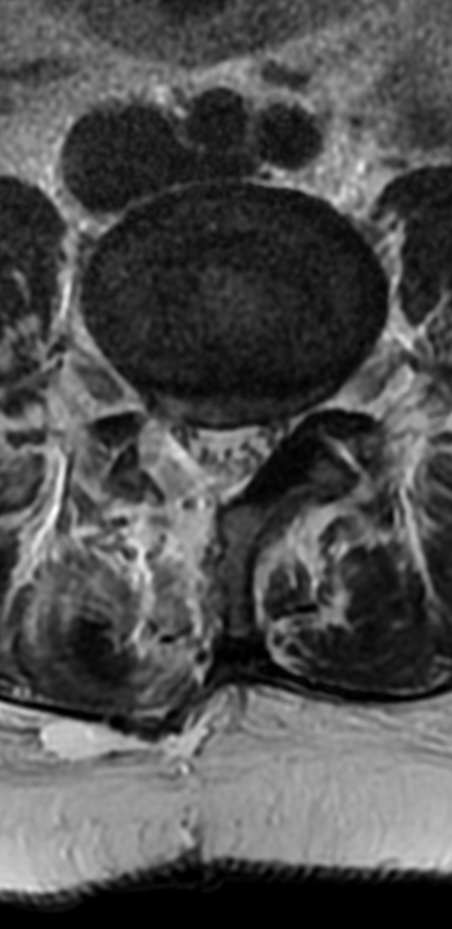
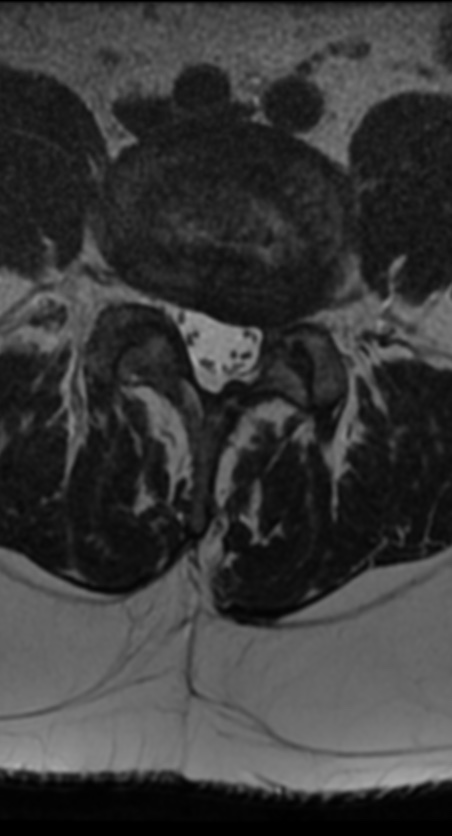
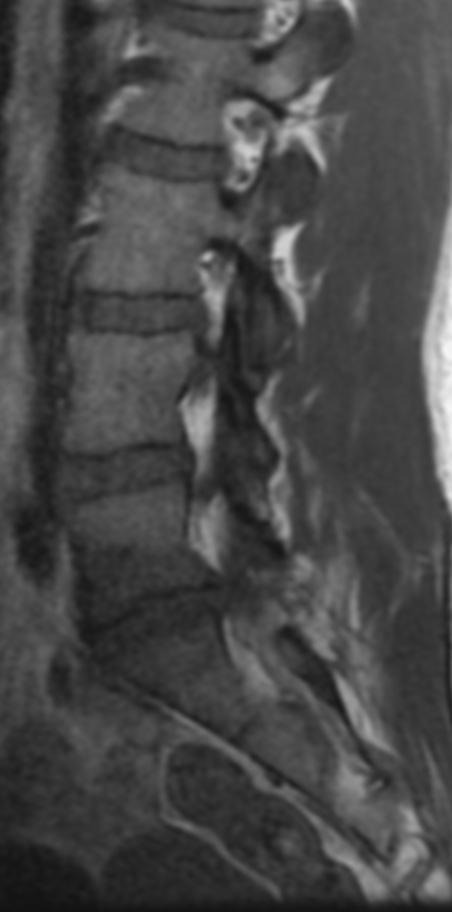
Although various factors contribute to the failure of disc surgery, recurrent disc herniation remains the major source of disability. Recurrent lumbar disc herniation has been reported in widely varying incidences between 3% and 18% of the patients and depends on the duration of the follow-up. Recurrent disc herniation is a significant problem, as scar formation may lead to increased morbidity after traditional posterior reoperation. Furthermore, persistent low back pain or re-recurrent sciatica may develop in some cases after repeated surgery. Also, it is important to consider the possibility of iatrogenic instability during surgery on the lumbar spine for the treatment of recurrent disc herniation.
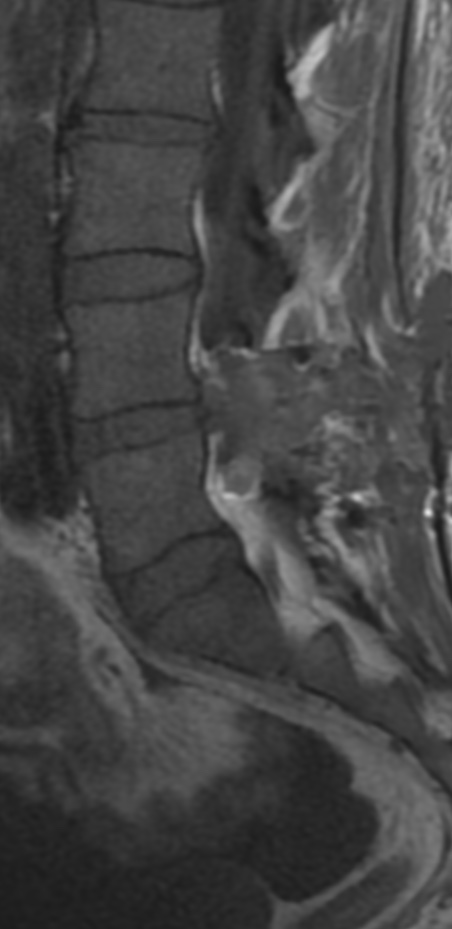
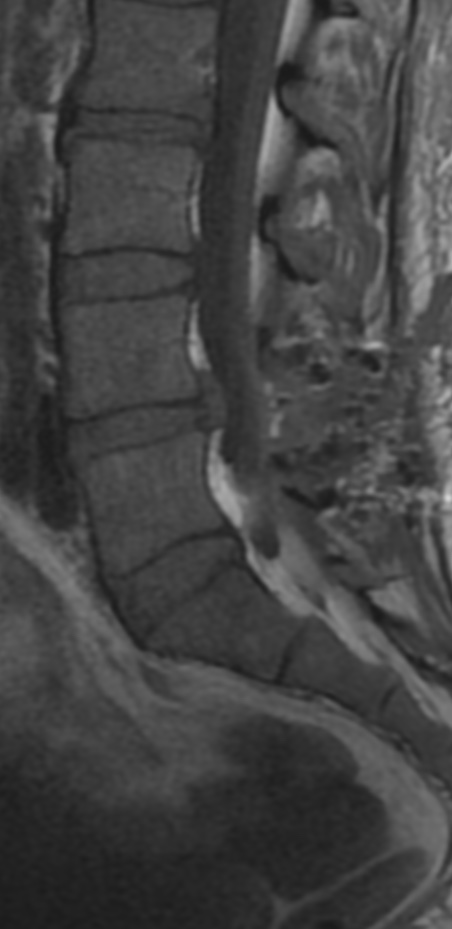
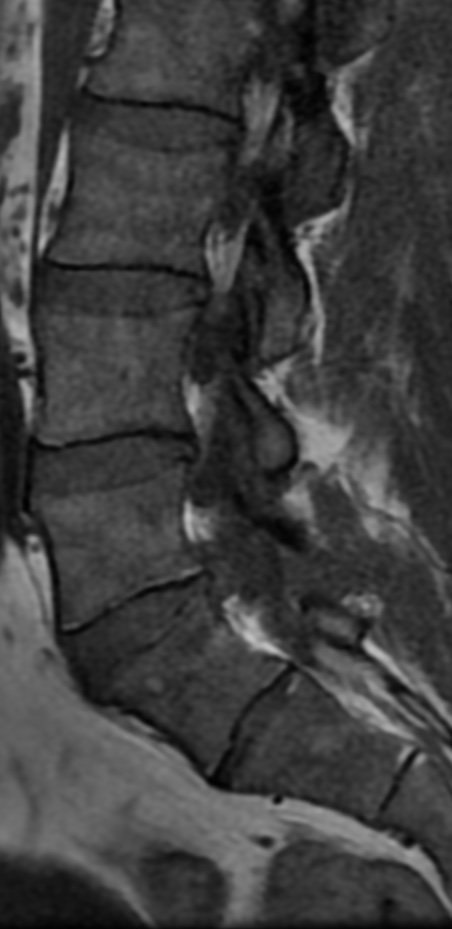
The optimal surgical technique for treating recurrent lumbar disc herniation is controversial. Some authors believe that in the absence of objective evidence of spinal instability, recurrent lumbar disc herniation may be adequately treated by repeated laminectomy and discectomy alone. While others believe that various factors contribute to the failure of repeated lumbar disc surgery and discectomy alone without fusion remains the major source of disability.
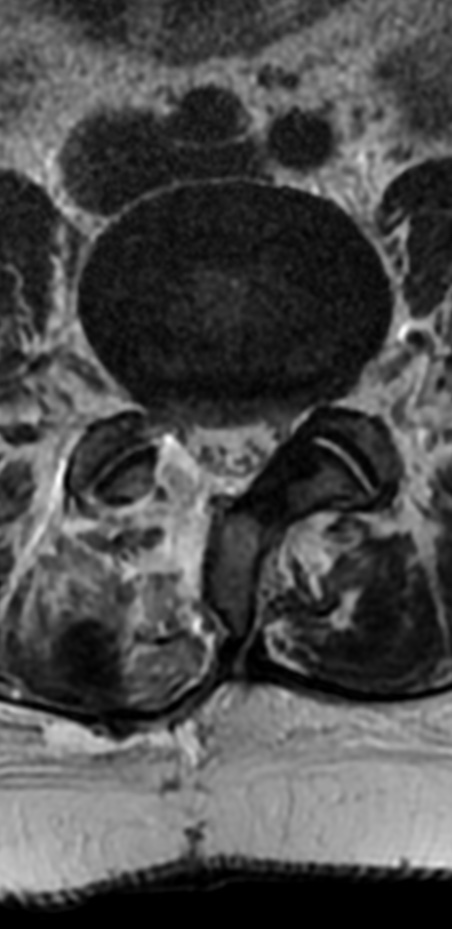
Fusion with repeated lumbar discectomy can be broadly categorized as posterolateral fusion (PLF) and interbody fusion. Various techniques for interbody fusion have been described, including anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF), and transforaminal lumbar interbody fusion (TLIF).



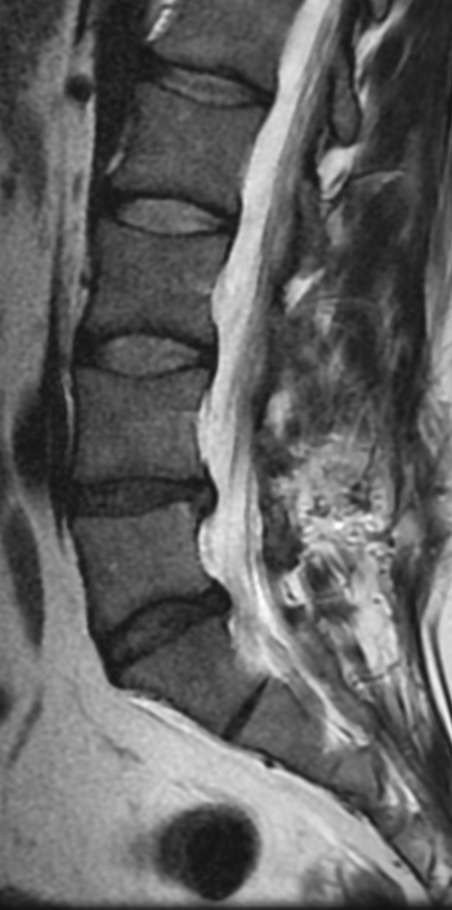


Revision discectomy is effective in patients with recurrent lumbar disc herniation with satisfactory rate up to 88.9%. Fusion with revision discectomy improves the postoperative low back pain, decreases the intraoperative risk of dural tear or neural damage and decreases the postoperative incidence of mechanical instability or re-recurrence. TLIF and PLF have comparable results when used with revision discectomy, but PLF has significantly less total cost than TLIF.





References: