Otogenic brain abscess may occur as a complication of acute and chronic suppurative otitis media. Radiologists and Otolaryngologists should have a high index of suspicion for otogenic abscesses in patients with a history of chronic ear disease and new symptoms of fever, headache, and nausea.
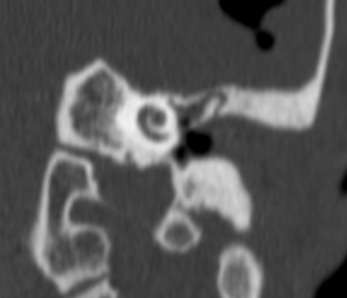
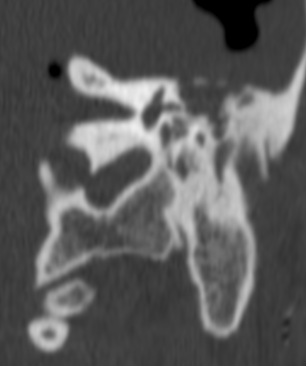
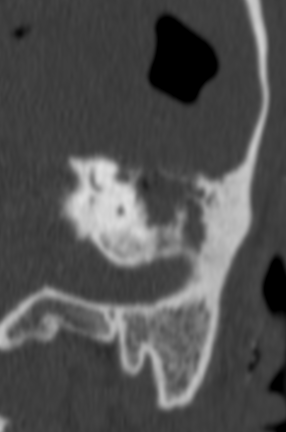
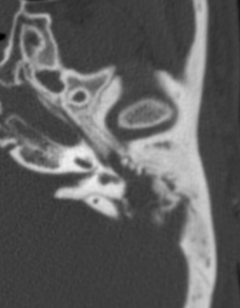
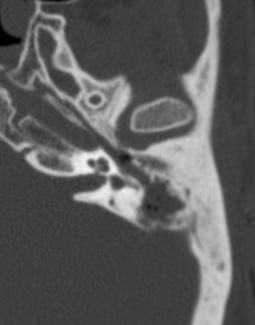
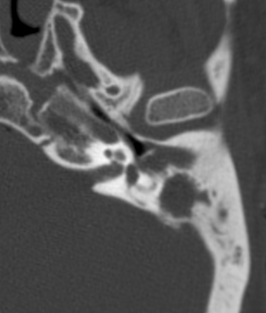
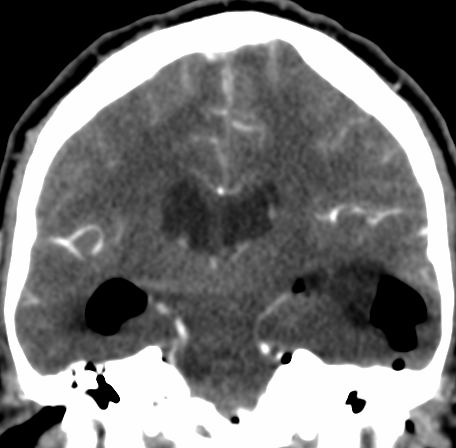
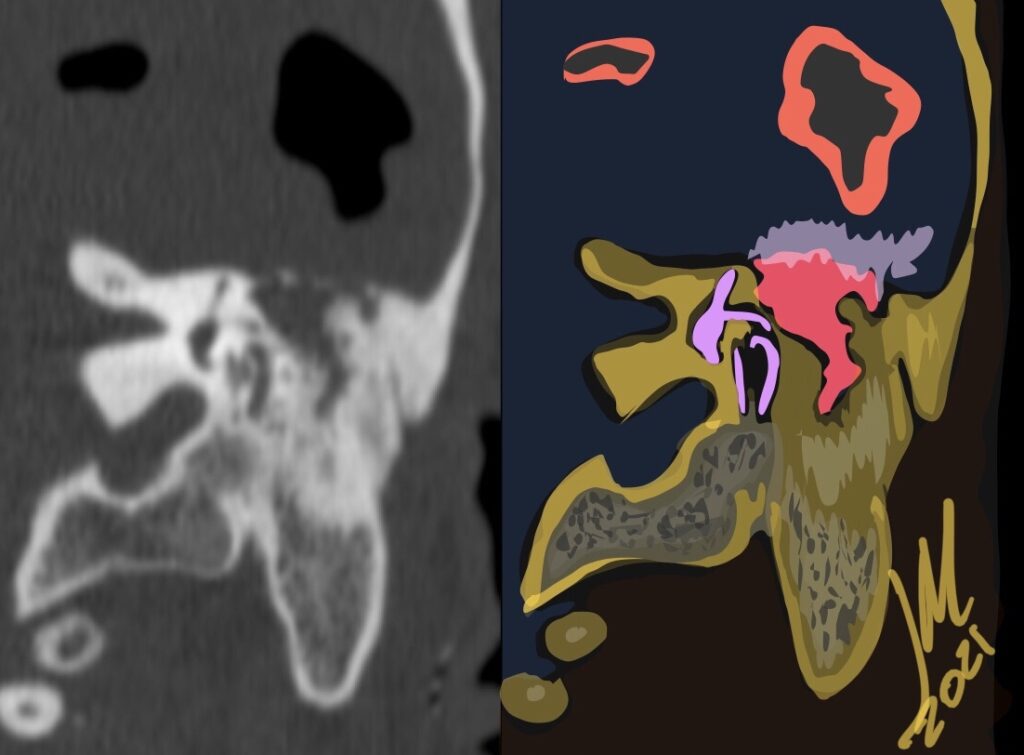
Otitis media (OM) is a common otologic condition in pediatric and adult populations. Acute mastoiditis (AM) is a complication of otitis media in which infection in the middle ear cleft involves the mucoperiosteum and bony septa of the mastoid air cells. It can be divided into coalescent and non coalescent mastoiditis. In coalescent AM, infection causes osteolysis of the bony septa or cortical bone, which can further lead to intra and extracranial complications
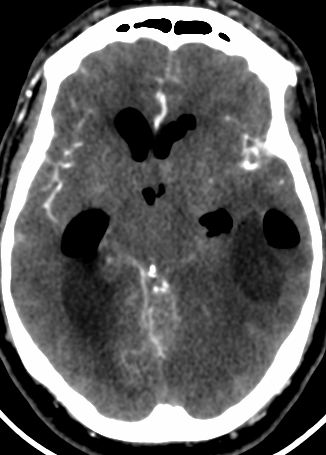
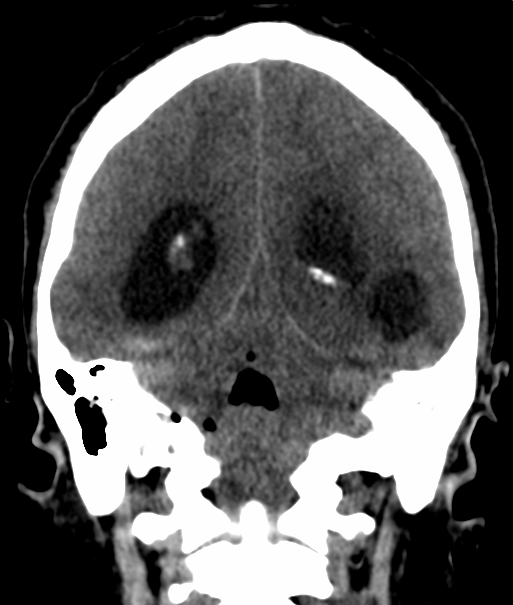
The imaging technique of choice is CT for its sensitivity in detecting opacification and bone destruction. Its capability to differentiate among causes of opacification is poor. MR imaging provides additional imaging markers reflecting soft-tissue reaction to infection, major intramastoid signal changes, diffusion restriction or intramastoid, periosteal, or dural enhancement as well as brain abscess.
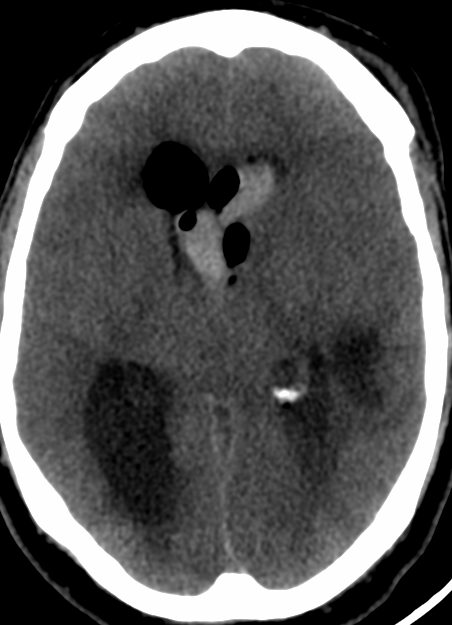
Complications of OM are classified as extracranial or intracranial. Brain abscess are commonly considered the second most common intracranial complication of OM after meningitis. Historically, it has been reported that 25% of brain abscesses in children were otogenic, whereas in adults it is thought that more than 50% of brain abscesses were otogenic.