
Myxopapillary ependymoma is a distinct subtype of spinal cord ependymomas that has a predilection for the lumbosacral region.
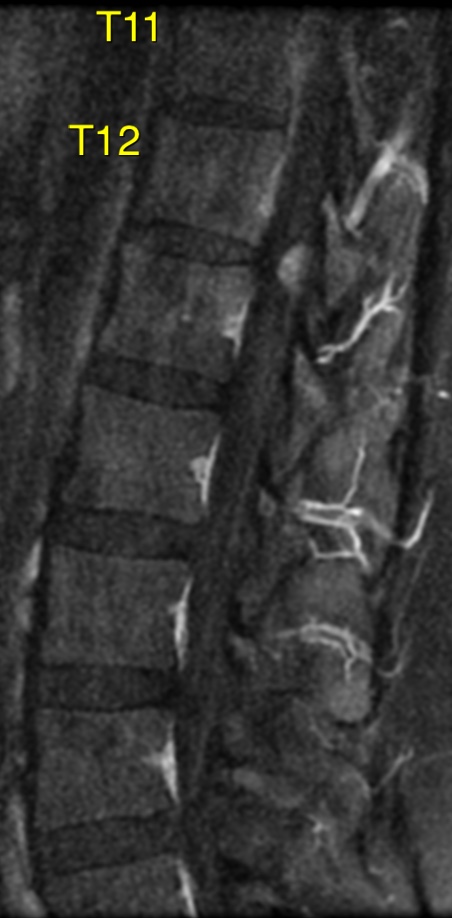
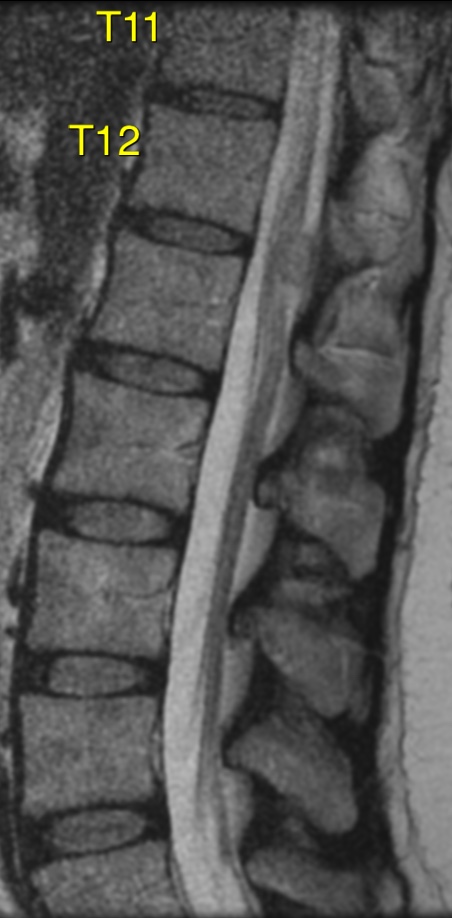
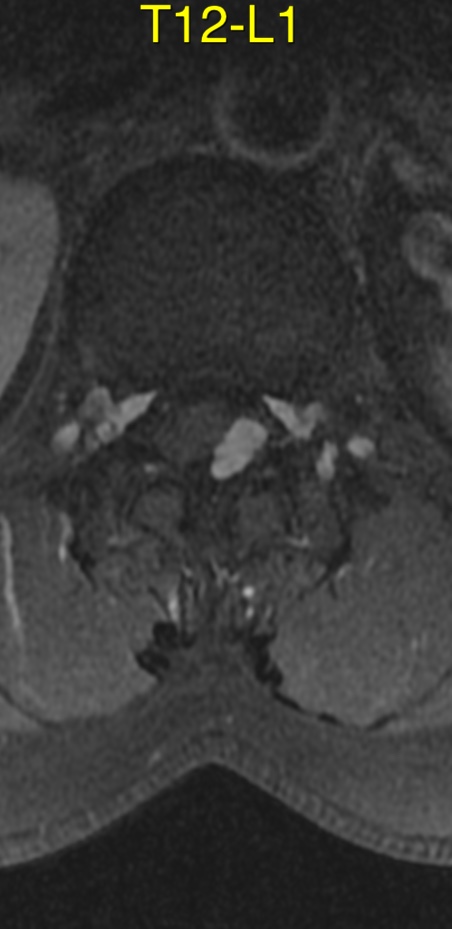
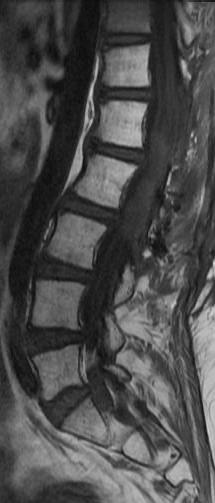
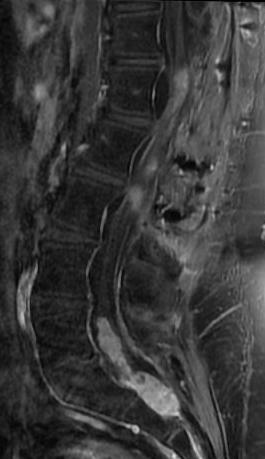
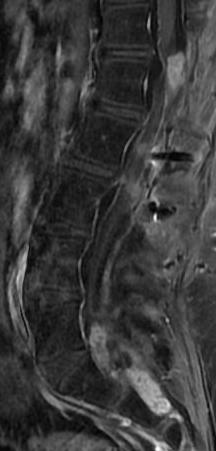
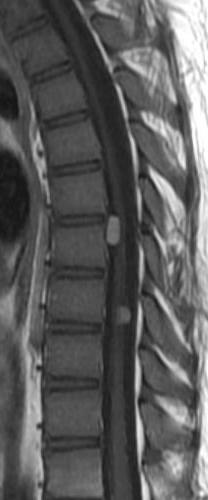
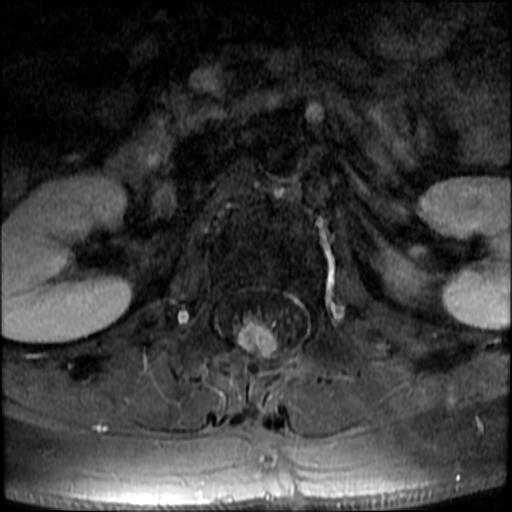
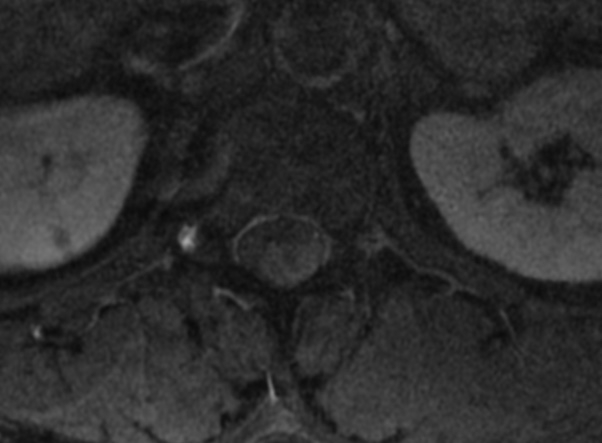
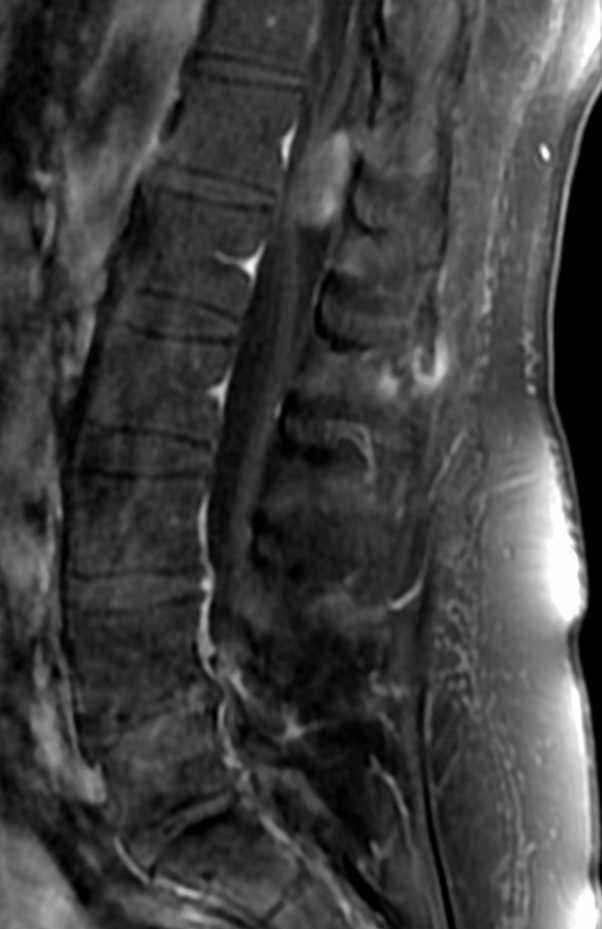
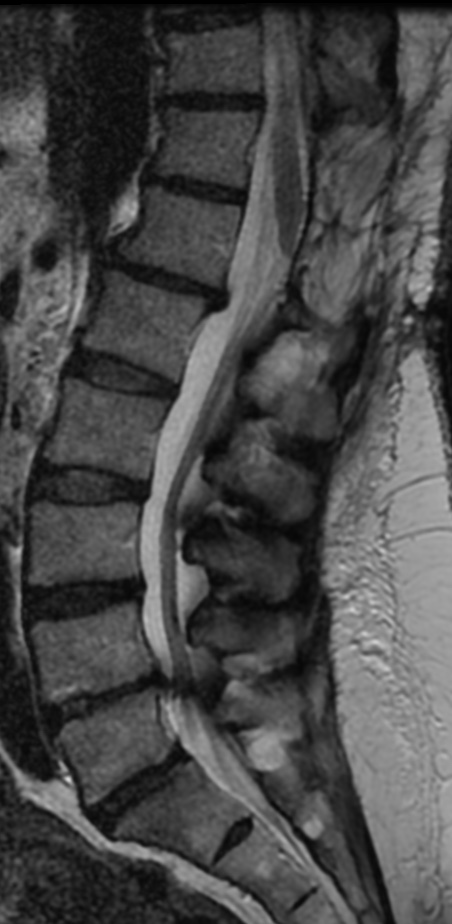
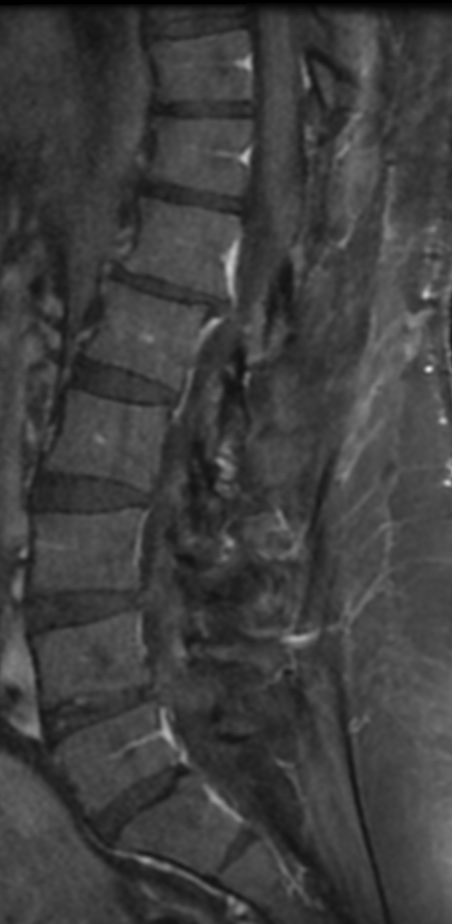
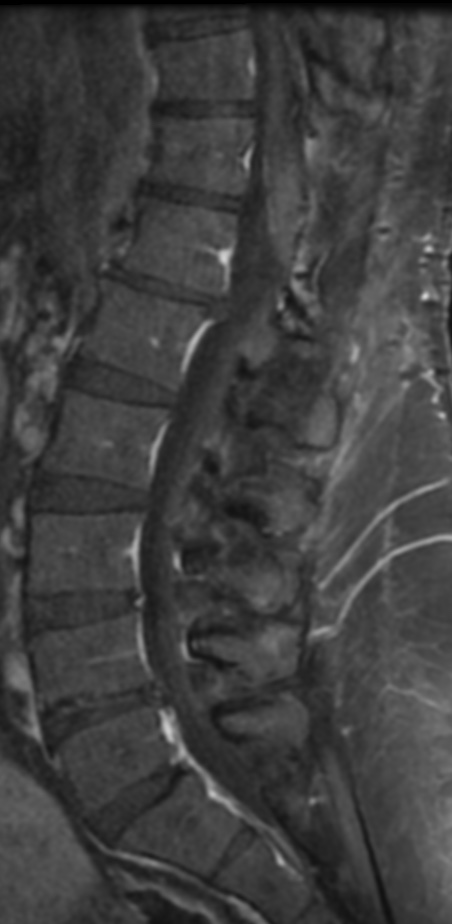
Magnetic resonance imaging is helpful in identifying the extent of the tumor and its relationship to intraspinal structures. It also allows for visualization of the cauda equina both above and below the tumor and will identify drop metastases in the subarachnoid space. Such information is useful in preoperative surgical planning. Magnetic resonance imaging findings in myxopapillary ependymomas are nonspecific.
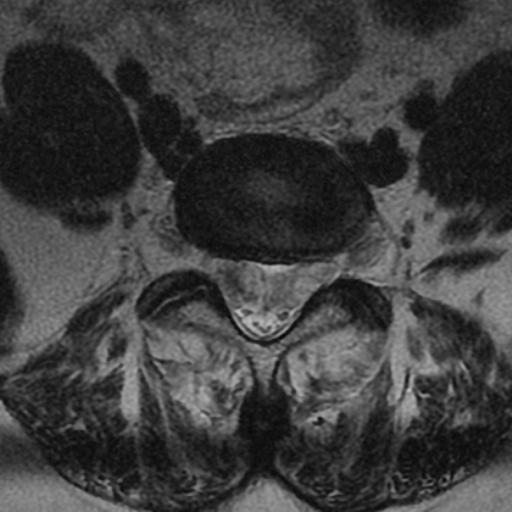
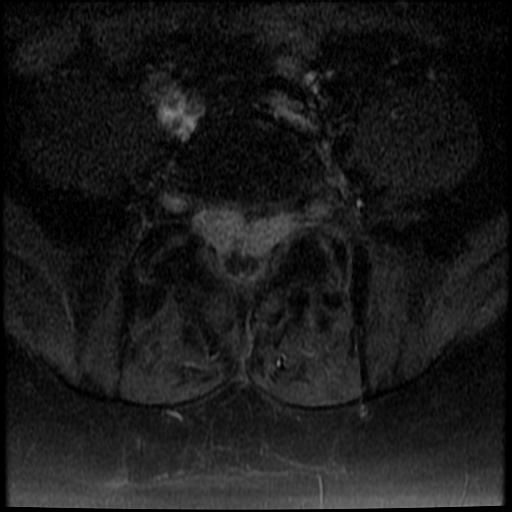
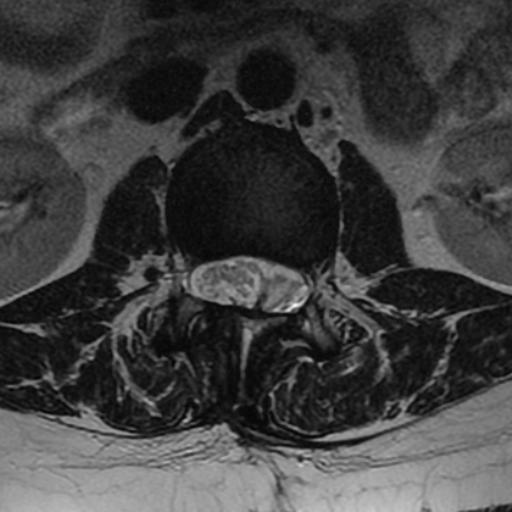
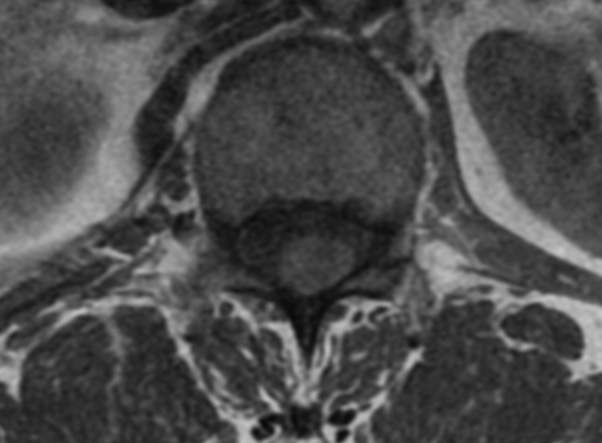
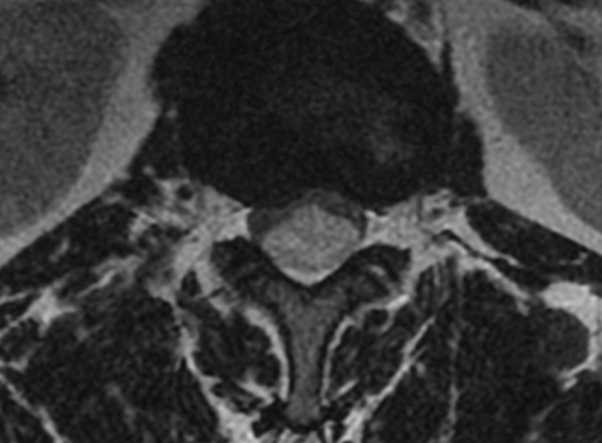
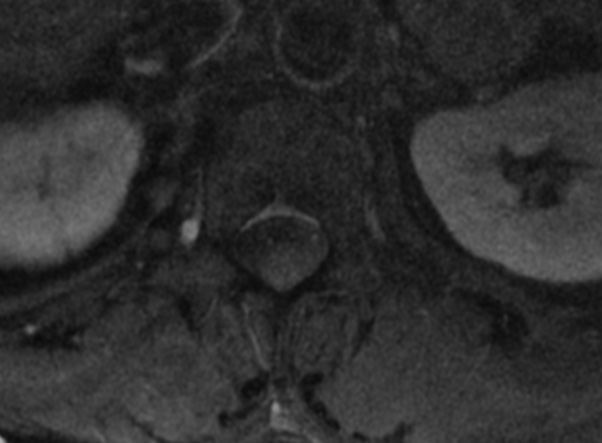
On magnetic resonance imaging, the lesion is iso- to hypointense on T1 and hyperintense on T2. Owing to their mucin content, the signal is hyperintense in myxopapillary ependymoma. Moreover, the tumor is heterogeneous after gadolinium injection. Hemorrhage and cyst formations are common features that contribute to signal inhomogeneity.
However, these tumors do contain certain features that help suggest the diagnosis. These features include:
- An intradural extramedullary thoracolumbar mass
- The tumor extends for several vertebral levels in the lumbar and sacral canal.
- It is hypointense to isointense on T1-weighted images.
- It is hyperintense on T2 weighted images.
- There will be an intense, homogeneous enhancement after the administration of contrast.
- There will usually be a region of slightly lower intensity at tumor margin on T2-weighted sequences.
- Cystic rostral or caudal degeneration exists in 50% of cases.
- Ependymomas of the brain frequently calcify, calcification is extremely unusual in spinal ependymoma.
The differential diagnoses of filum terminale and small conus myxopapillary ependymomas include:
- Fibrous meningioma:The fibrillary variant of myxopapillary ependymomas may be confused with fibrous meningioma
- Schwannoma: The fibrillary variant of myxopapillary ependymomas may be confused with schwannoma
It represents 13% of all spinal ependymomas and accounts for 90% of all tumors in the conus medullaris. Myxopapillary ependymoma is a benign and slow-growing neoplasm.




Myxopapillary ependymomas are considered benign tumors of the central nervous system with long-term survival rates and a tendency for local recurrence. However, an aggressive course has occasionally been described, leading to cerebrospinal fluid dissemination and even systemic metastases.
Myxopapillary ependymoma arises from the ependymal glia of the filum terminale. No risk factors for the development of this tumor have been described. Extradural myxopapillary ependymomas are thought to arise from the coccygeal medullary vestige or the extradural remnants of the filum terminale.
Myxopapillary ependymomas account for 1% to 5% of all spinal neoplasms and approximately 13% of all spinal ependymomas. In the American population, their incidence was 1.00 per million person-years. The age at onset varies between 30 and 50 years (mean age, 35 years). The most common location of myxopapillary ependymoma is the lumbosacral spine segment, mainly in the conus medullaris and cauda equina regions. Other rare locations include the cerebral ventricles and the brain.




Early detection and treatment of patients affected by myxopapillary ependymomas are crucial to achieving optimal patient outcomes. The best treatment modality for myxopapillary ependymoma is complete surgical resection, which is associated with a complete resolution for the majority of patients. Surgery should be performed early so as to guarantee better postoperative outcomes. Complete resection of this tumor may be hazardous, principally if the tumor involves the conus medullaris or is interlaced with the nerve roots of the cauda equina. Surgeons must be very careful since nerve roots may also penetrate directly through the tumor.
Reference: