
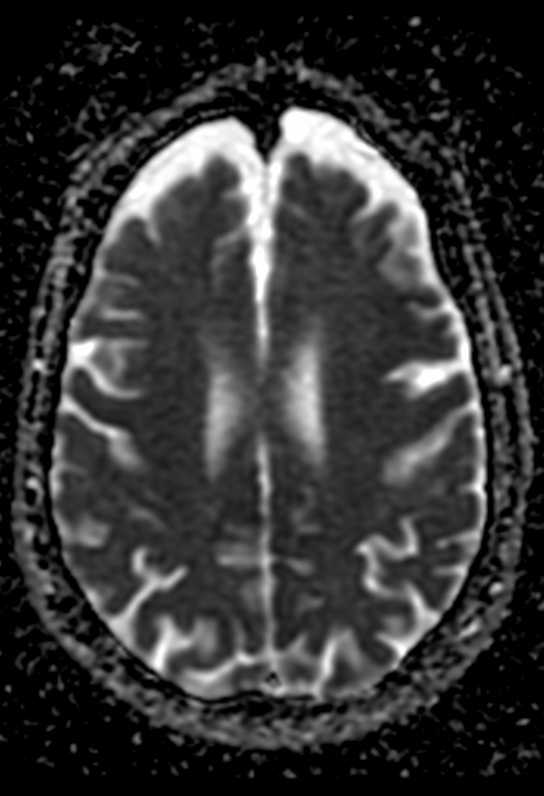
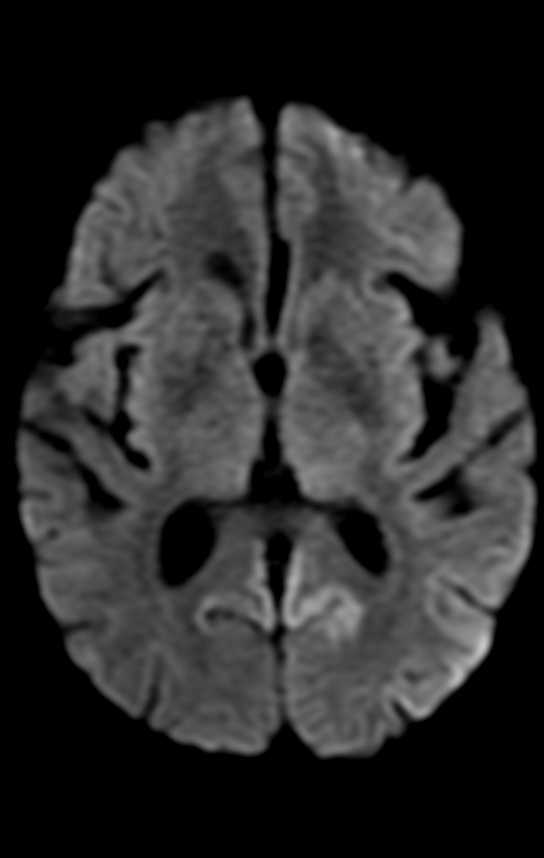
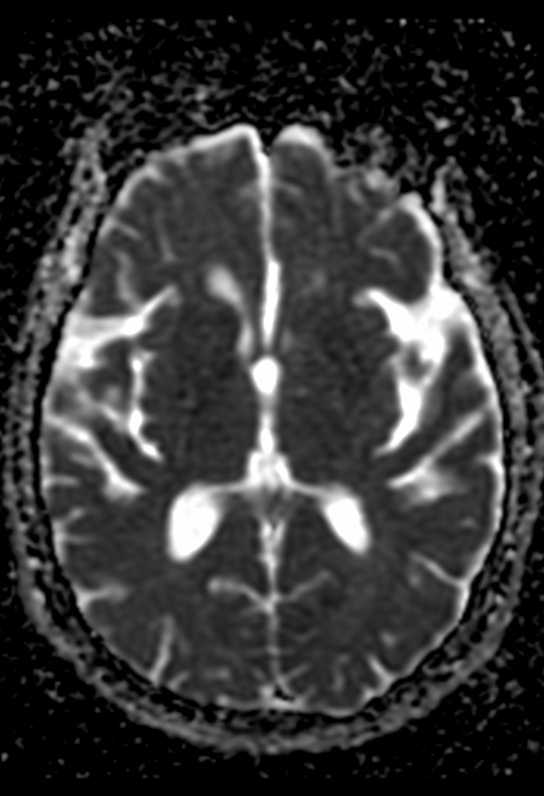
On MR imaging, the earliest changes are seen on DWI sequences. The involved regions show restricted diffusion with corresponding ADC hypointensity. The extent of these abnormalities depends on severity and duration of hypoglycemia.
Changes are usually bilateral, though bilaterally asymmetric, or, rarely, unilateral lesions, may occur. Reduction in ADC values has been shown to follow establishment of cerebral isoelectricity, a process that may be asynchronous. This may explain asymmetric lesions in a given patient.
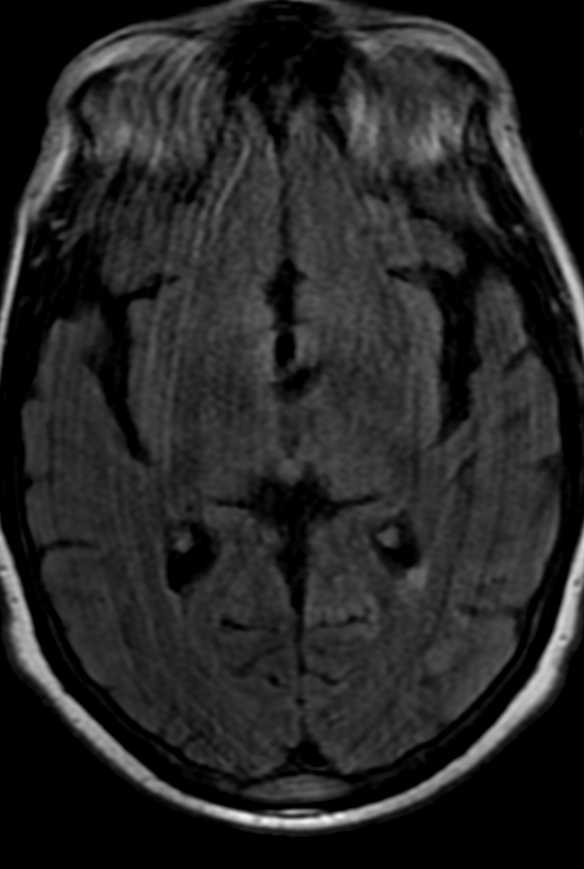
On the basis of the topographic distribution of the signal abnormalities, 3 imaging patterns have been described. These include 1) predominant gray matter involvement affecting the cortex, neostriatum, and hippocampi; 2) predominant WM involvement affecting the periventricular WM, internal capsule, and splenium of corpus callosum and 3) mixed pattern, involving both the gray matter and WM.
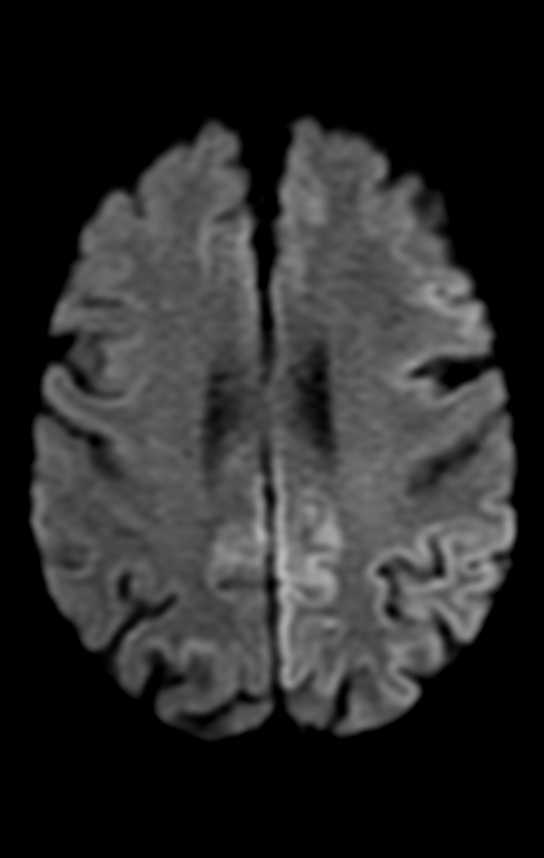
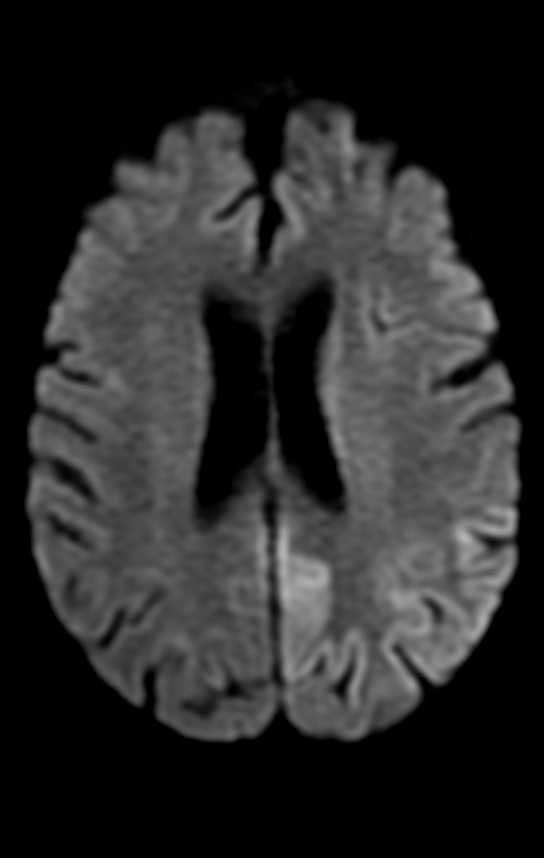
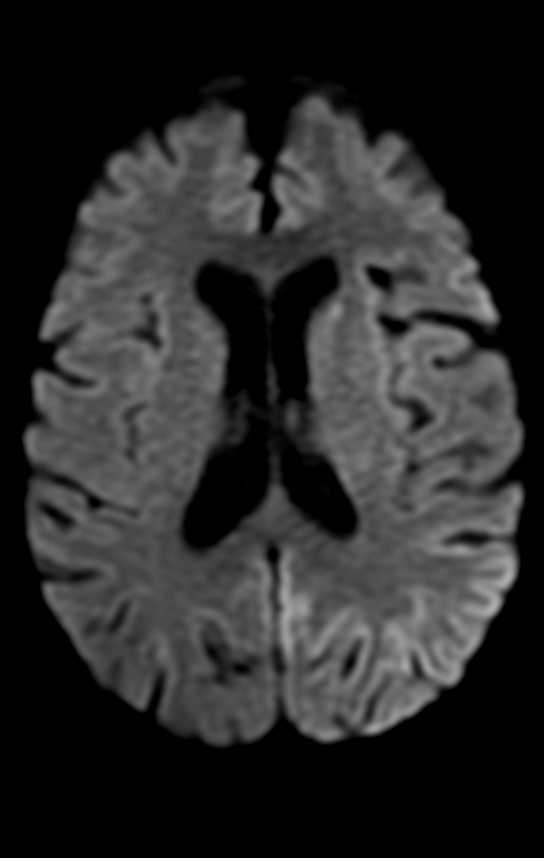
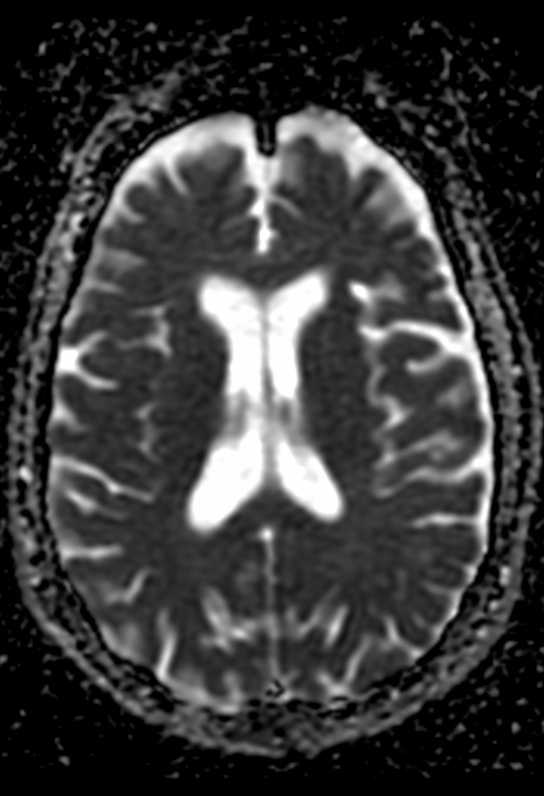

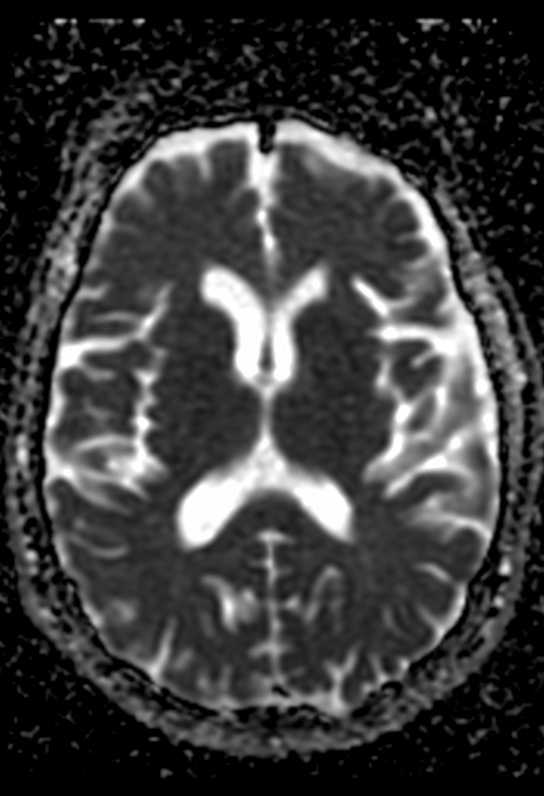
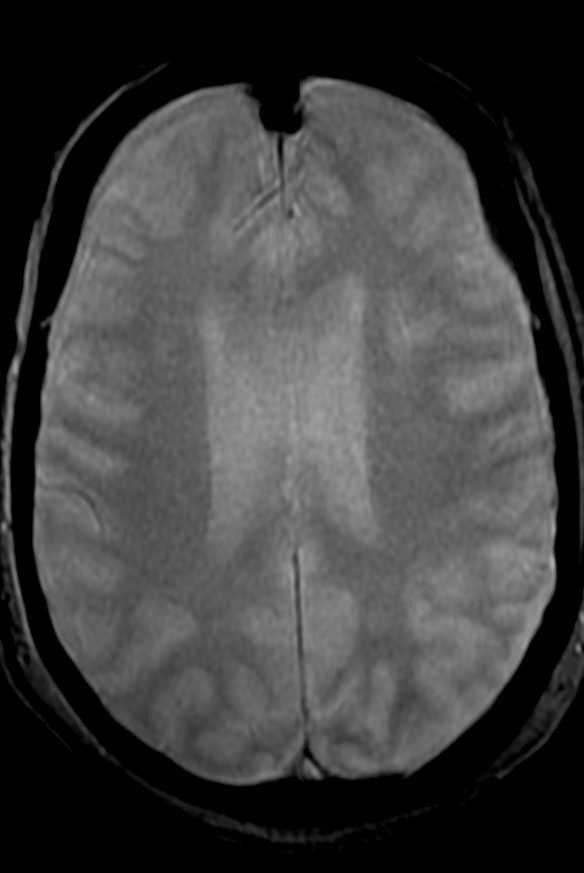
The division of patients on the basis of these imaging patterns is of unclear significance.Patients with focal involvement of the internal capsule, corona radiata, or splenium usually have a good prognosis. These lesions usually resolve promptly after restoration of blood glucose, though they tend to follow clinical symptom resolution. Resolution of DW abnormalities in their patient as early as 2 hours after blood glucose levels were restored.
Patients with extensive WM involvement show variable response. The prognosis in these cases varies between complete recovery and persistent vegetative state. Clinical improvement, if it occurs, is usually delayed by weeks. Involvement of the neostriatum and diffuse cortical lesions often portend dismal outcome. Failure of lesions to regress on follow-up imaging is also associated with poor prognosis.
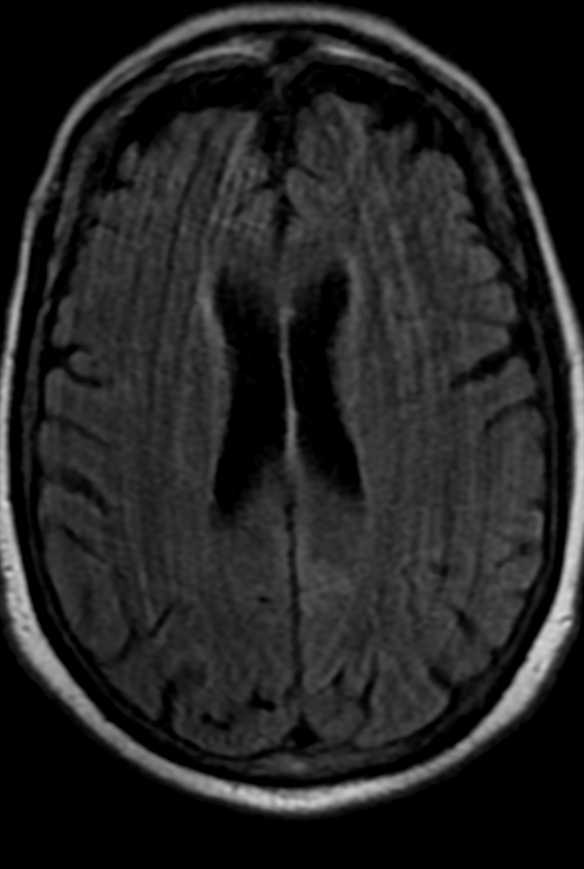
Findings of CT scans of the head on admission were often unremarkable in the reported cases, but in time, some acute-stage and chronic-stage changes have been demonstrated. In the acute stage, the changes varied from subtle decreased attenuation of the basal ganglia to diffuse brain edema, as severity of the hypoglycemia increased. In the chronic stage, diffuse brain atrophy and dilation of the ventricular system have been noted. MR imaging findings are comparable to the CT findings, mainly involving the cortex, internal capsule, basal ganglia, and hippocampus.
Diffusion-weighted MR imaging detects change in water diffusion with cellular dysfunction and primarily identifies early ischemic changes in stroke. Infarction is the most common cause of such a hyperintense lesion on diffusion-weighted imaging. In hypoglycemia, the incidence of cytotoxic edema, shrinkage of the extracellular space as a result of hypoglycemia, and failure of the ionic pumps cause the hyperintense lesion on diffusion-weighted MR imaging. ADC reductions similar to those seen after ischemia occur in hypoglycemia, status epilepticus, spreading depression, and excitotoxic brain injury, pathologic conditions characterized by a significant shrinkage of the extracellular space volume. However, status epilepticus and spreading depression in normal brain are conditions that are not associated with energy failure, and the ADC changes are reversible. Glucose deprivation leads to severe brain energy failure and a reduction of cell membrane ionic pump activity, as does anoxia/ischemia, but the topographic and temporal evolution of hypoglycemic brain damage is different from that of anoxia/ischemia.
Hyperacute short-term severe hypoglycemia for <10 minutes does not induce visible changes in DWI of the human brain, suggesting that prolonged hypoglycemia may be the relevant cause for observed reversible diffusion disturbances in MR imaging. Therefore, prompt adequate therapy for hypoglycemia can prevent cerebral injury in patients with diabetes.
Hypoglycemia was initially reported to predominantly involve the cortex, neostriatum, and hippocampus. However, many authors have also reported predominant WM involvement, mainly affecting the centrum semiovale, corona radiata, internal capsule, an splenium of the corpus callosum. In fact, involvement of the WM is now thought to be earlier and more common than gray matter involvement. Some cases may show diffuse gray matter and WM involvement. The thalamus, brain stem, and cerebellum are invariably spared, and this may help to differentiate hypoglycemia from hypoxic injury, which often involves the thalamus.
Hypoglycemia is more common in diabetic patients and can occur as a complication of therapy with insulin or long-acting sulfonylurea drugs. Other causes include exogenous administration of insulin, which may be suicidal or accidental, insulin-secreting tumors, sepsis, Addison disease, and hepatic or renal failure.
Reference:
doi: 10.1097/MD.0000000000008425