Idiopathic hypereosinophilic syndrome (HES) is a heterogeneous disorder characterized by prolonged eosinophilia without an identifiable cause, ultimately resulting in organ dysfunction.
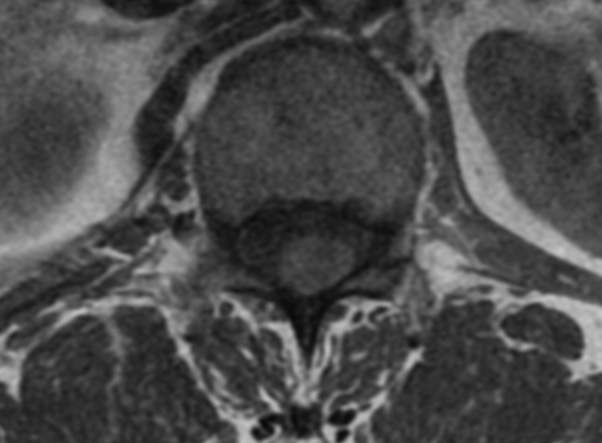
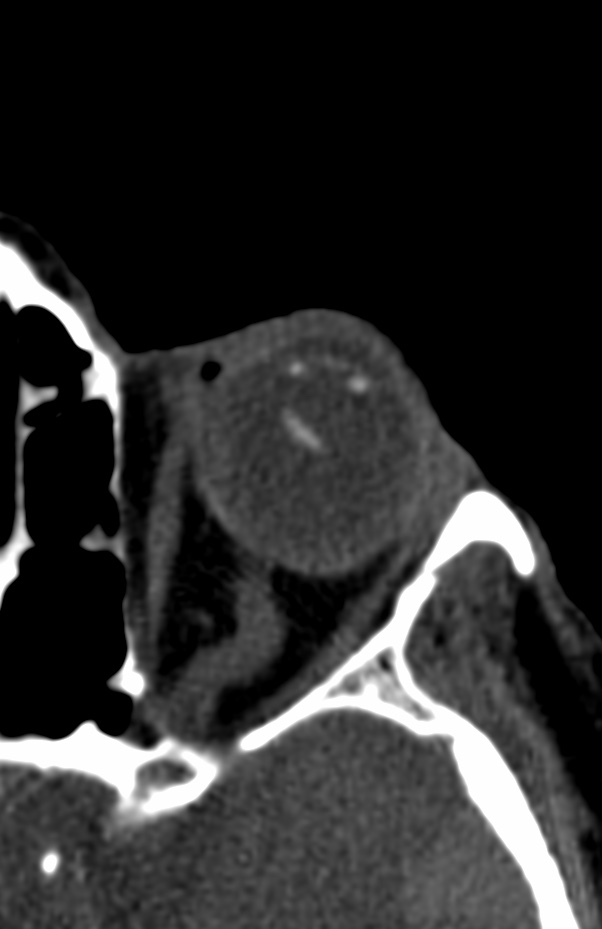
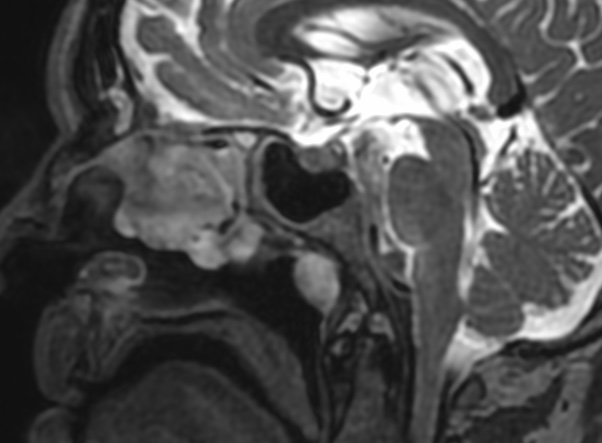
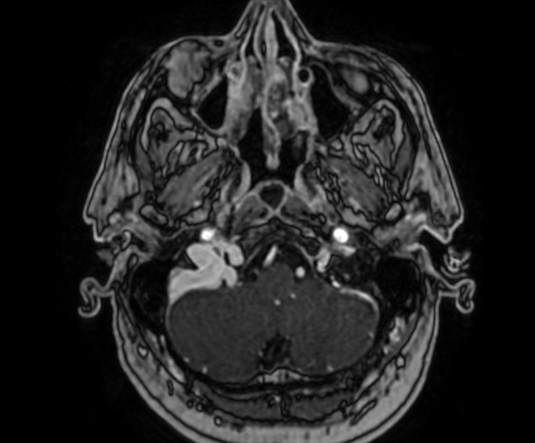
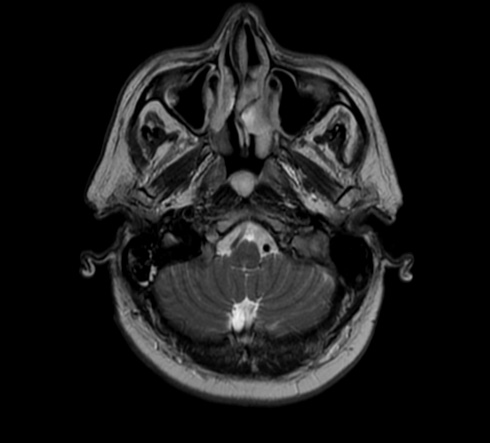
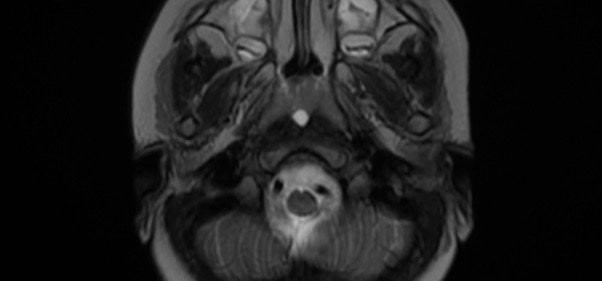
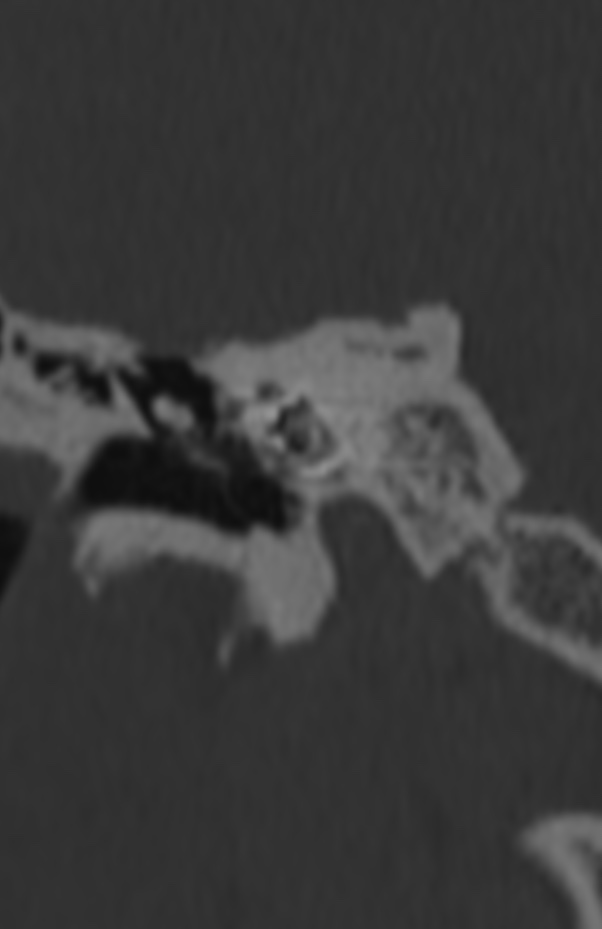
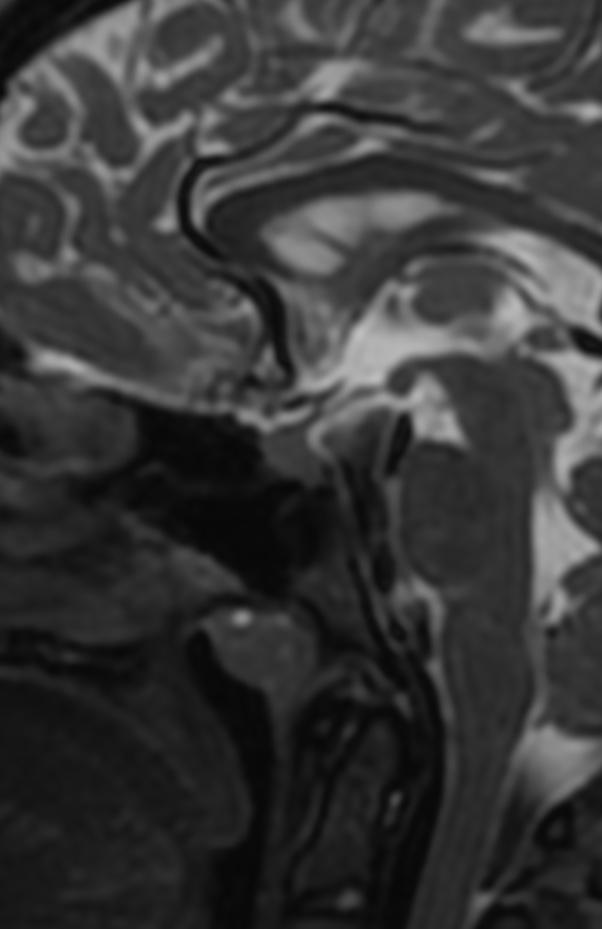
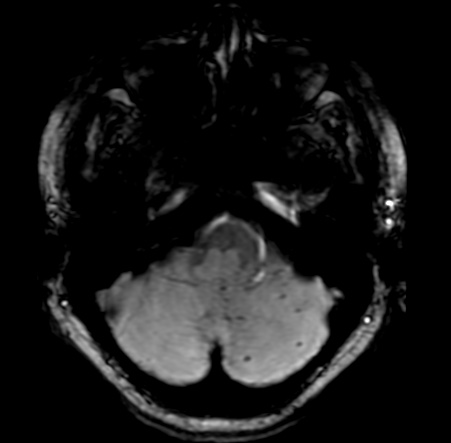
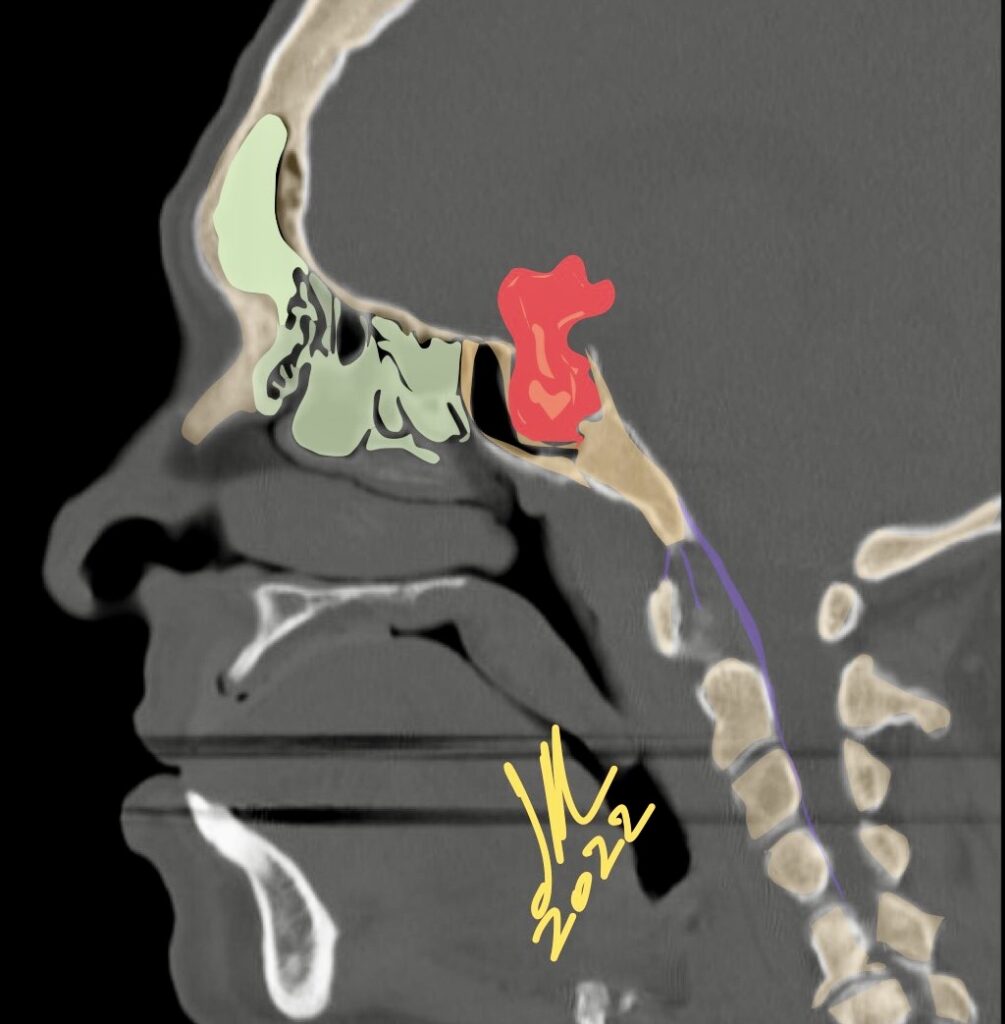
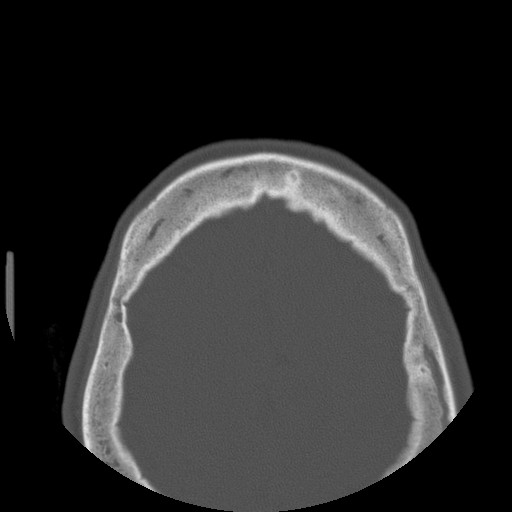
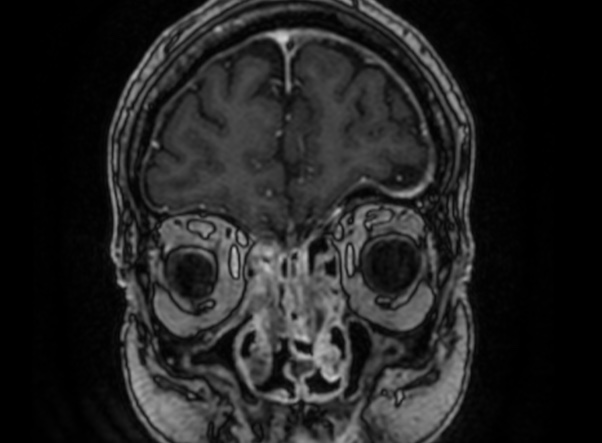
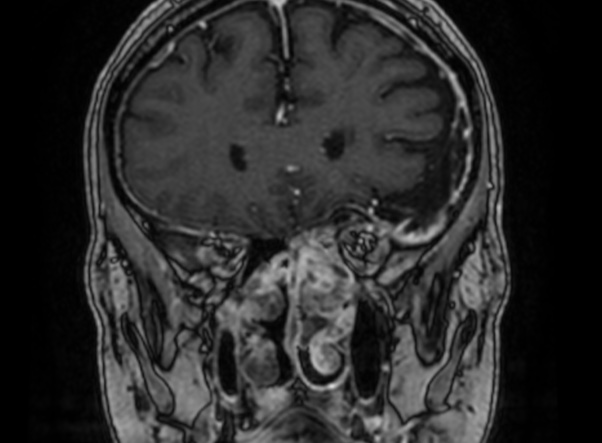
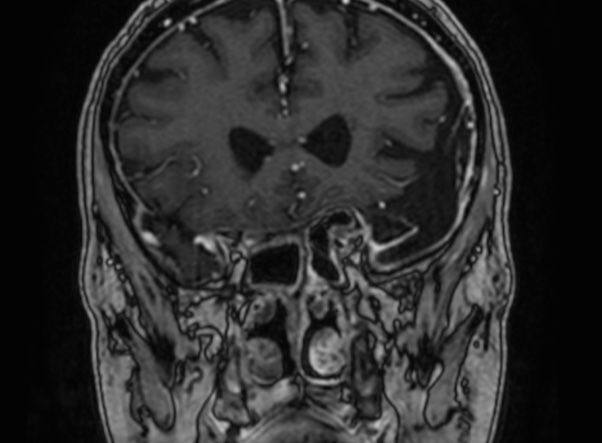
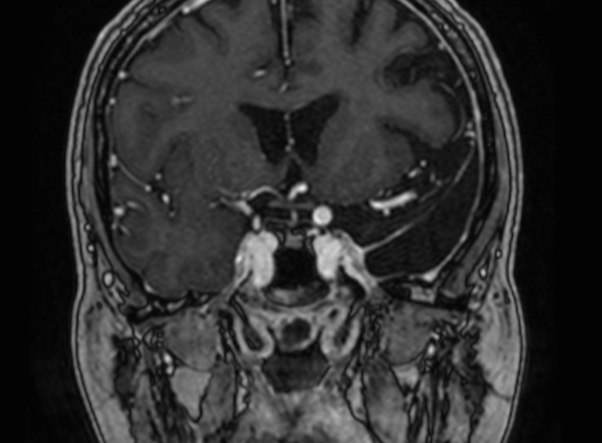
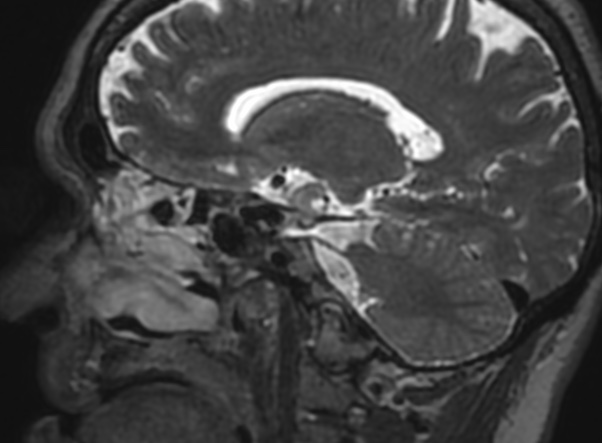
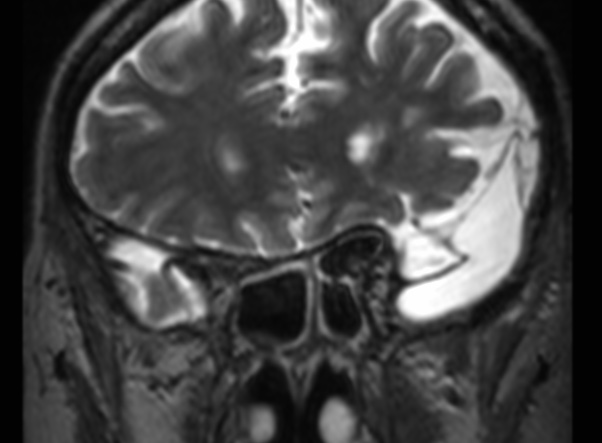
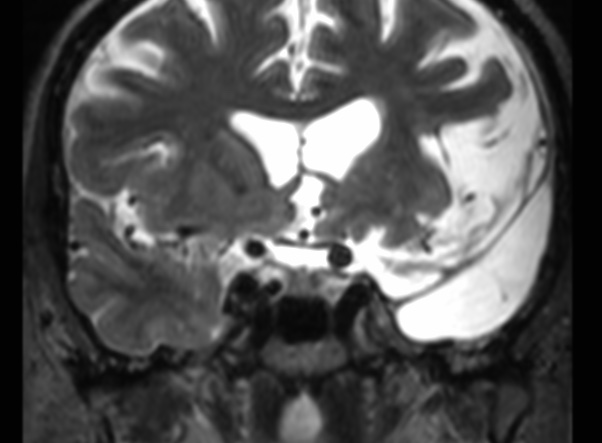
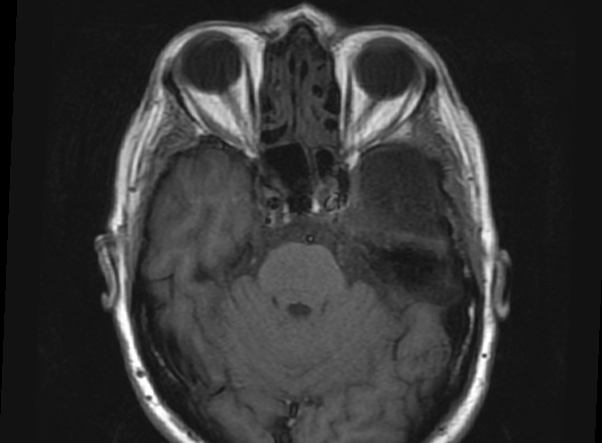
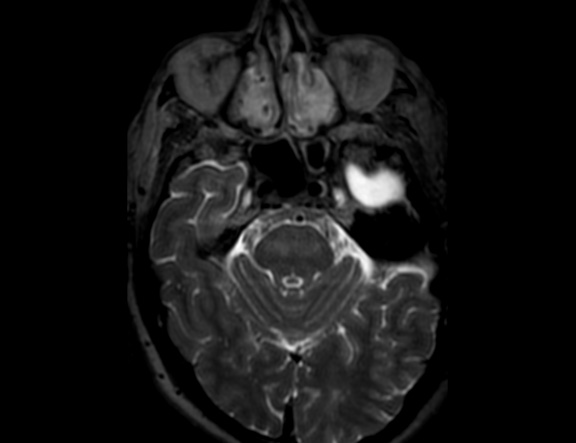
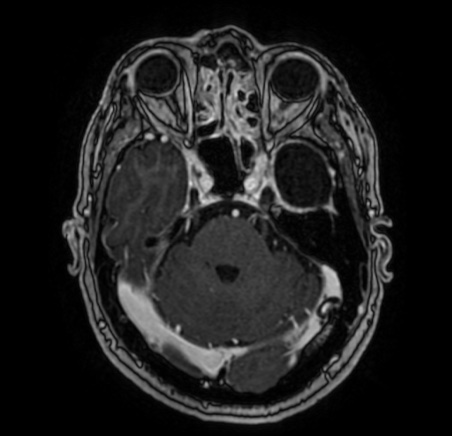
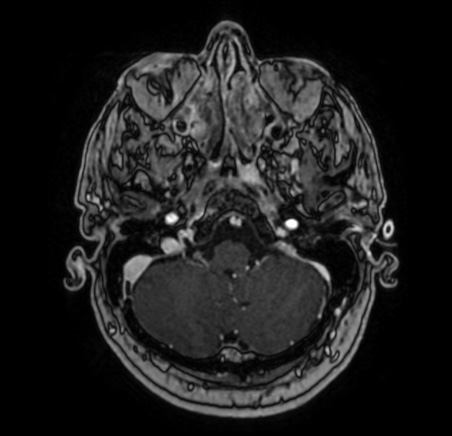
Idiopathic hypereosinophilic syndrome (HES) was first defined by Chusid et al in 1975 as unexplained eosinophilia of greater than 1500/μL present for longer than 6 months with evidence of organ injury related to the hypereosinophilia, such as cardiomyopathy, peripheral neuropathy, and encephalopathy. The heterogeneity of HES ranges from those patients with myeloproliferative features (splenomegaly, increased vitamin B12 levels, abnormal leukocyte alkaline phosphatase scores, and cytogenetic abnormalities) to those patients with benign courses (associated with increases in immunoglobulin E [IgE], angioedema, and corticosteroid-responsive eosinophilia). There is an unusual type of inflammatory pseudotumor (IPT) involving the skull base in a patient with HES who presented with multiple cranial nerve palsies.
It has a strong male preponderance, with a male-to-female ratio of 9:1, and most frequently involves the heart, lungs, nervous system, and skin.
In 1 series, 65% of patients with HES had neurologic involvement, and some reports have described recurrent optic neuritis as the presenting symptom of HES.
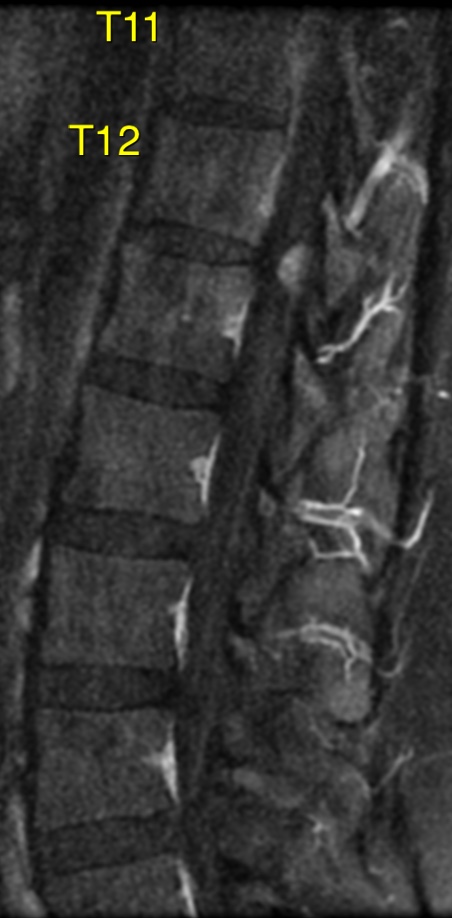
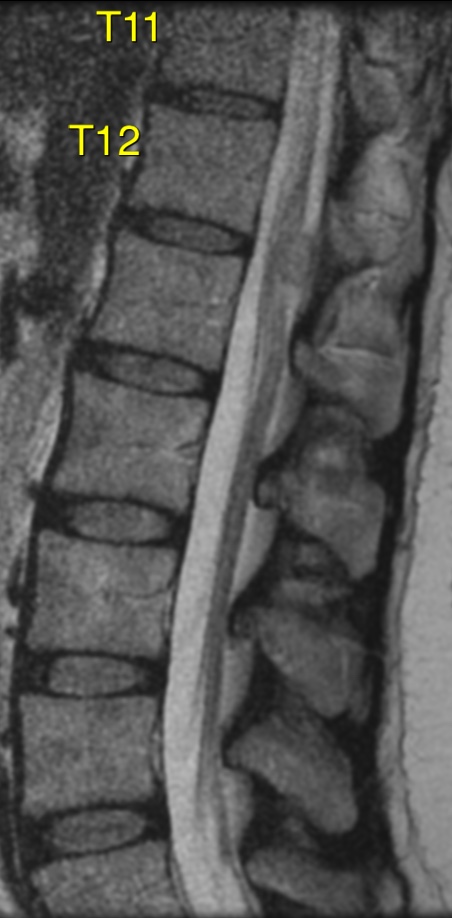
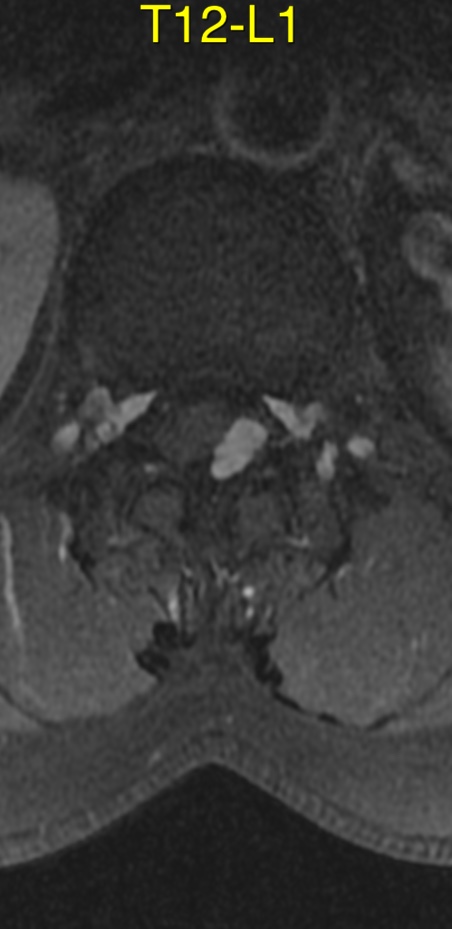
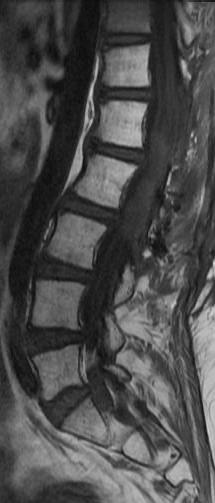
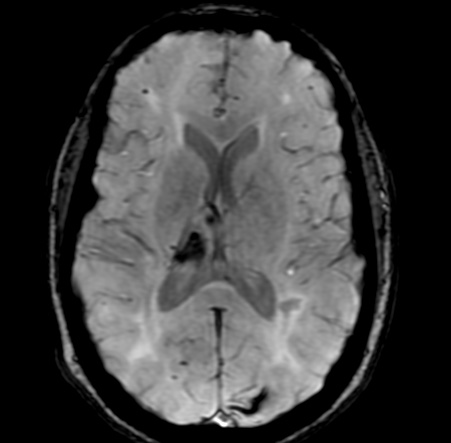
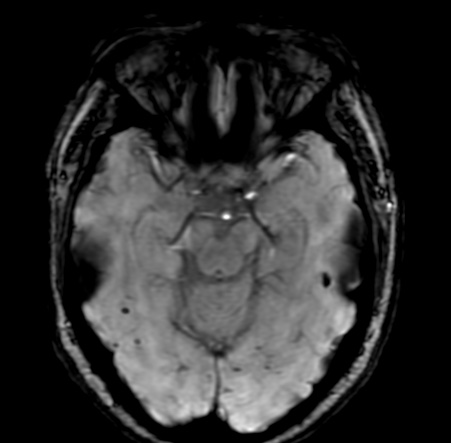
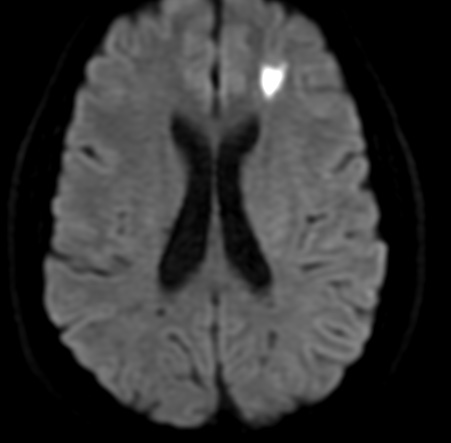
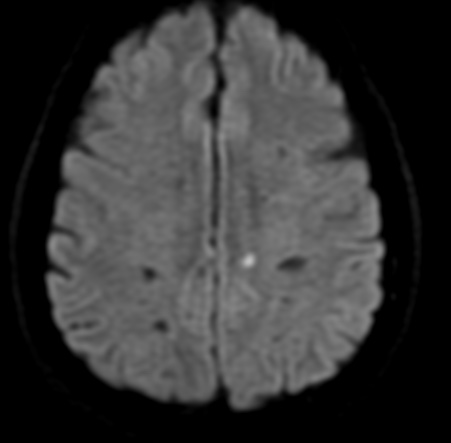
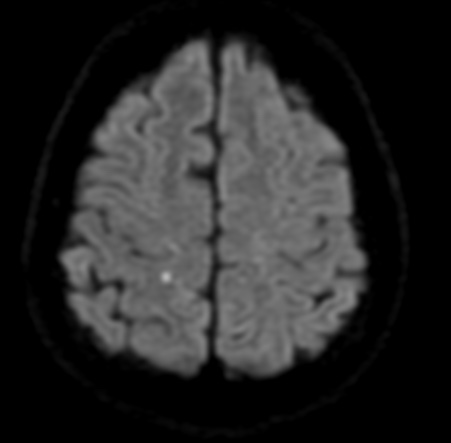
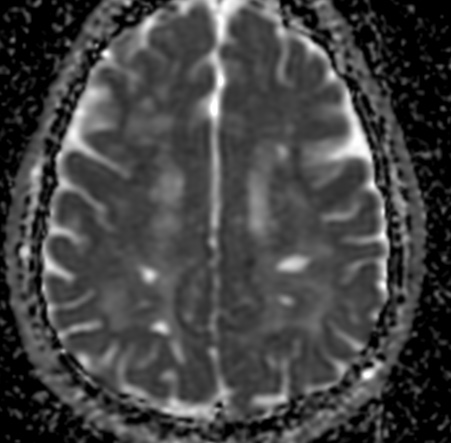
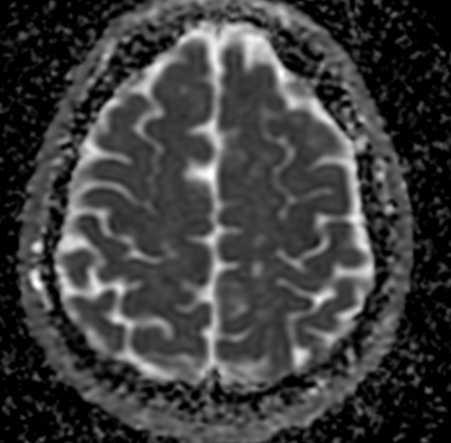
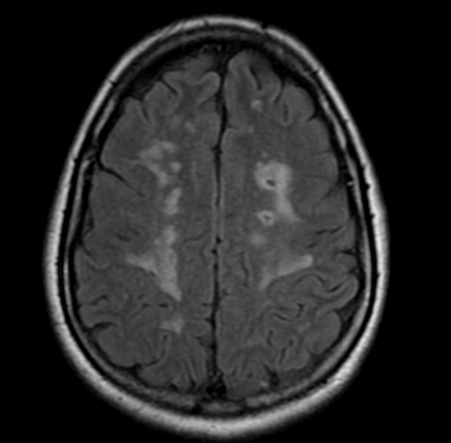
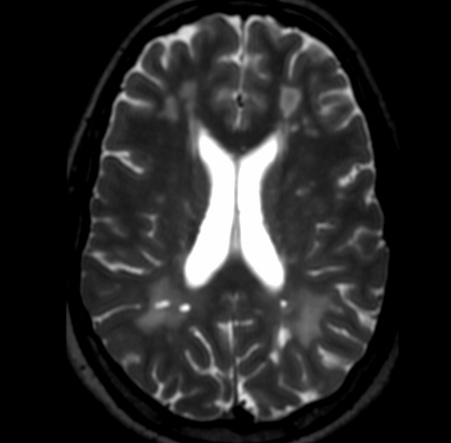
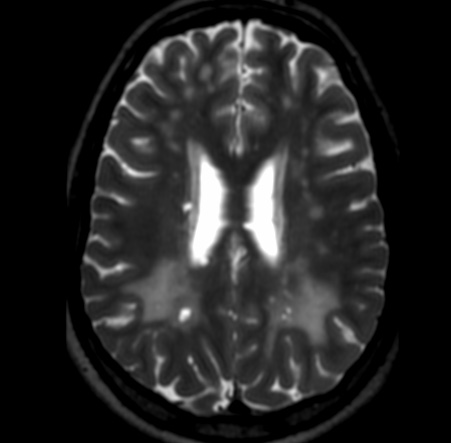
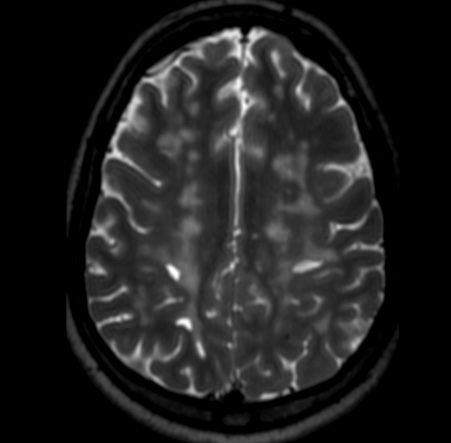
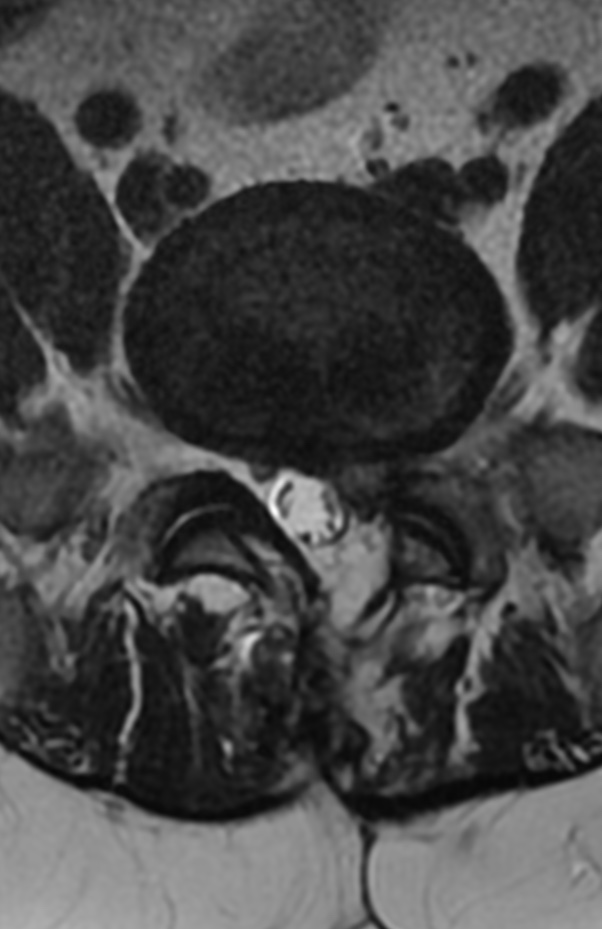
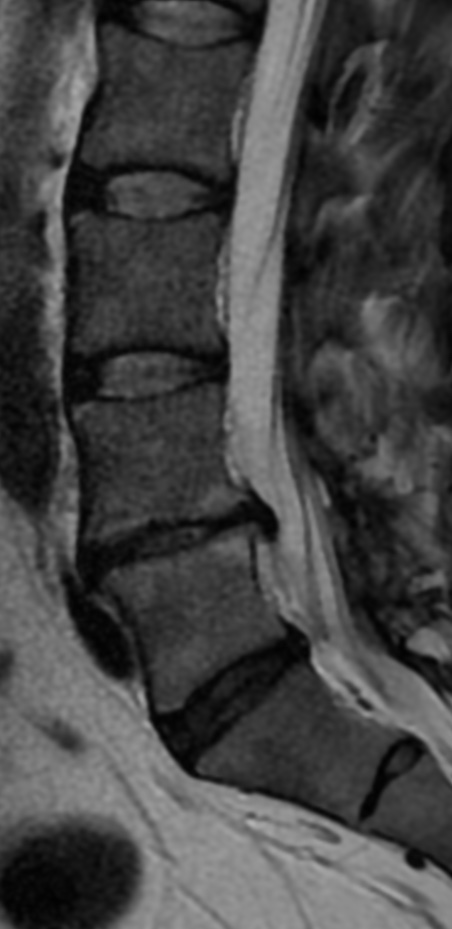
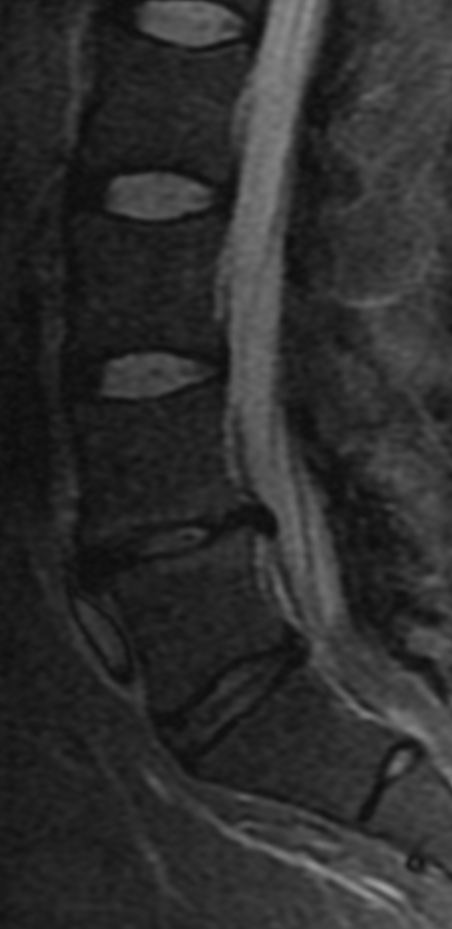
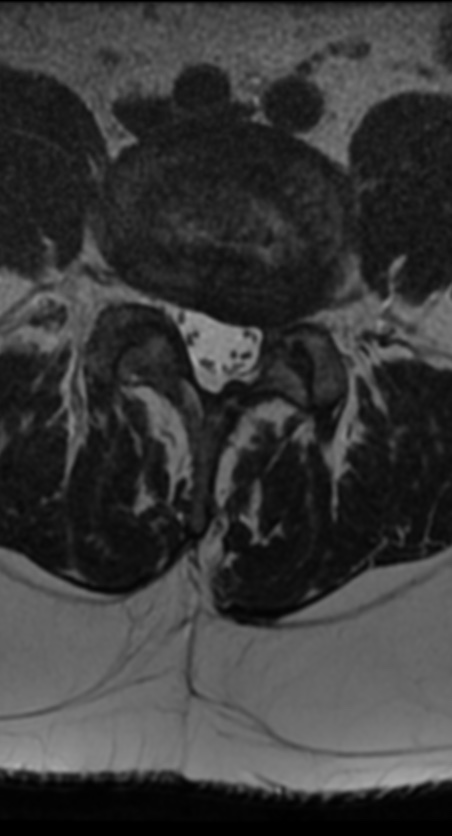
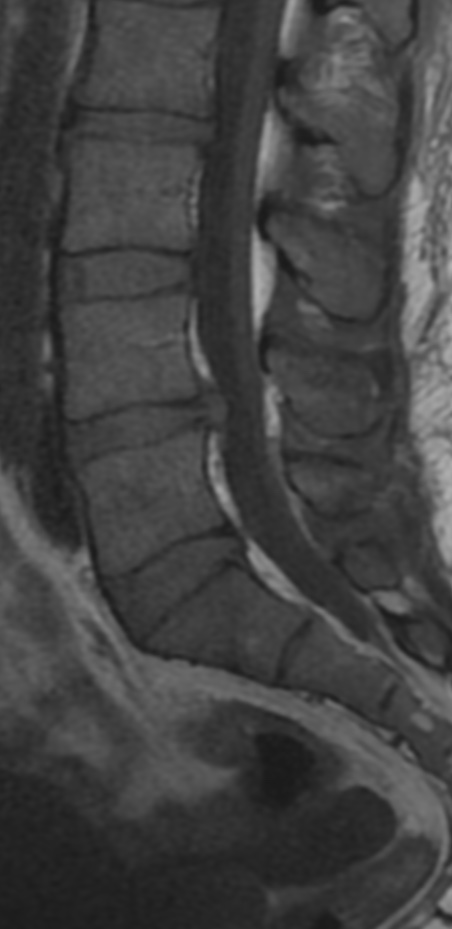
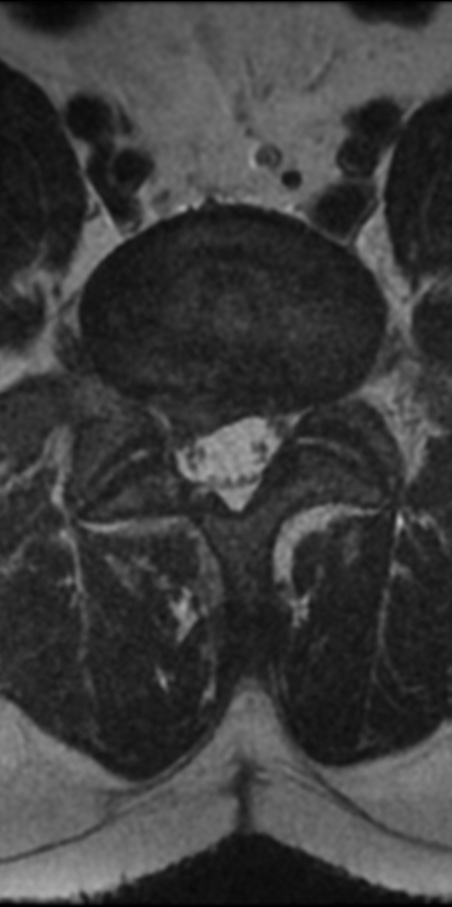
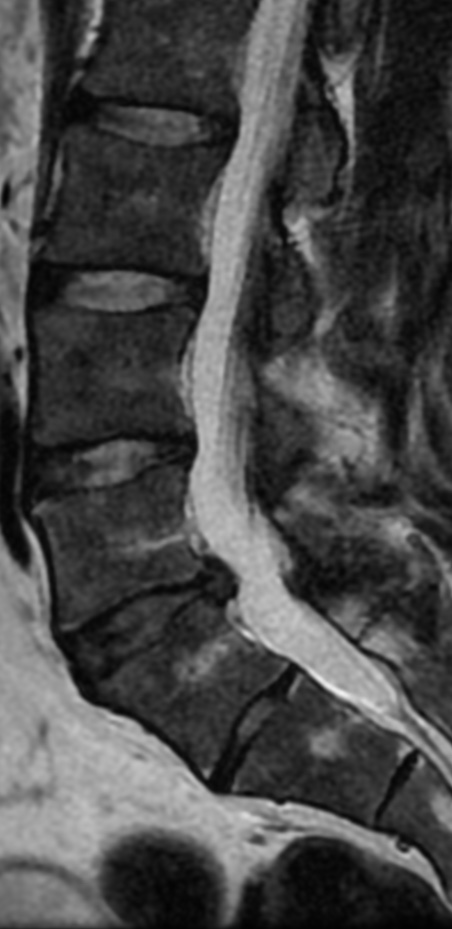
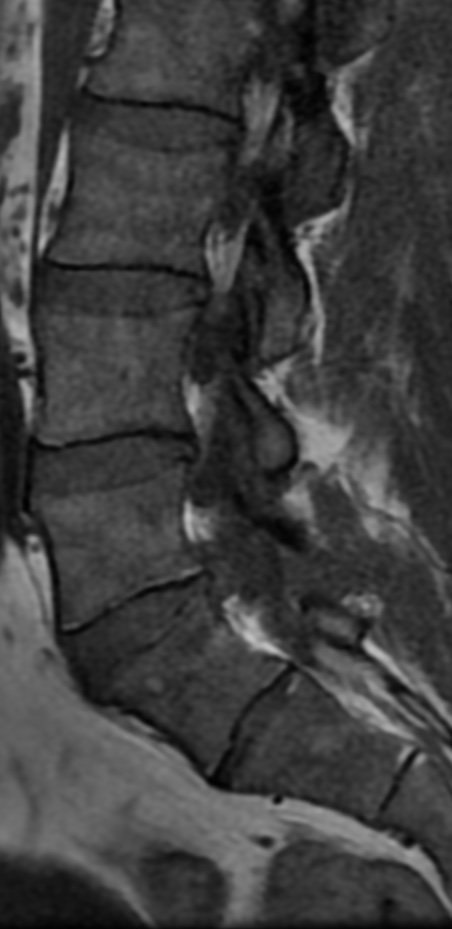
Three major types of neurologic involvement have been defined as follows: peripheral polyneuropathy, encephalopathy, and central nervous system (CNS) thromboemboli. Peripheral polyneuropathy is most common, occurring in approximately 50% of patients with HES, and may manifest as a sensory neuropathy, mononeuritis multiplex, radiculopathy, or muscle atrophy caused by denervation.
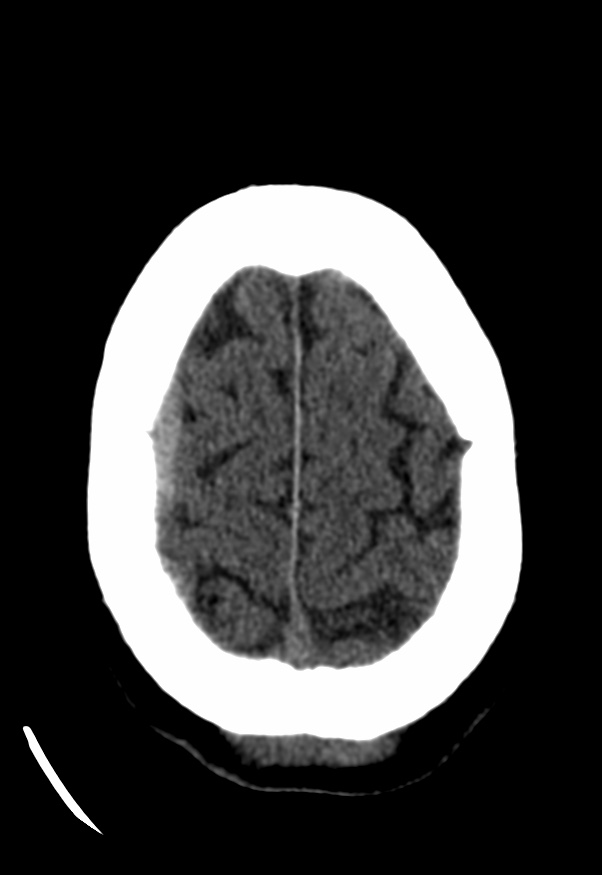
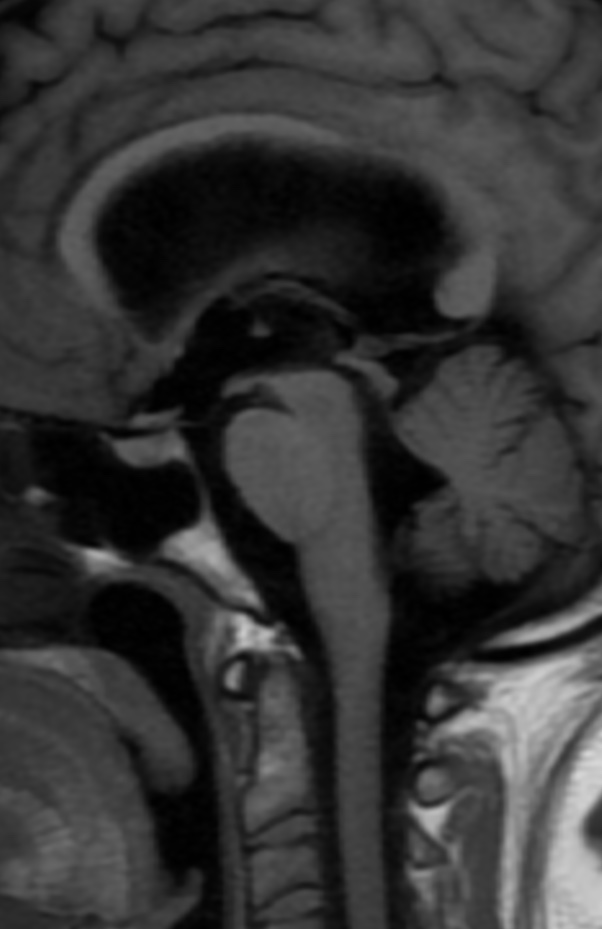
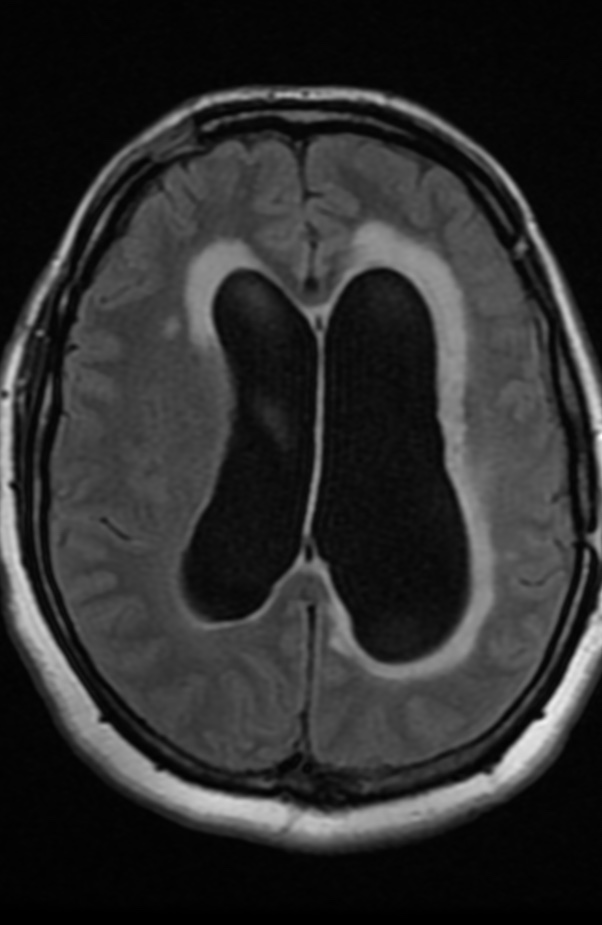
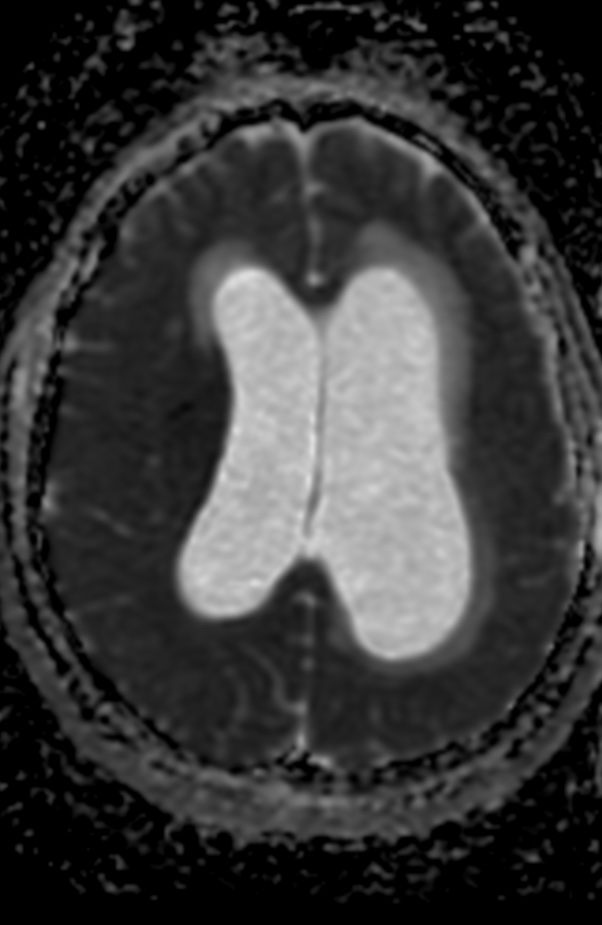
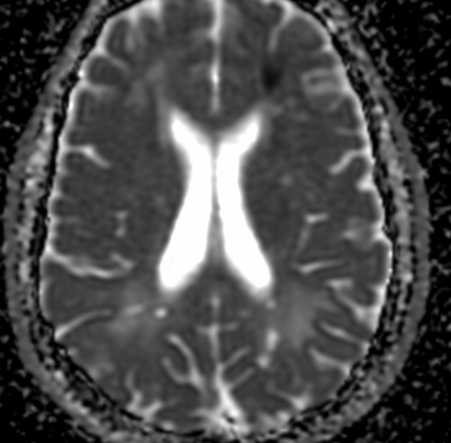
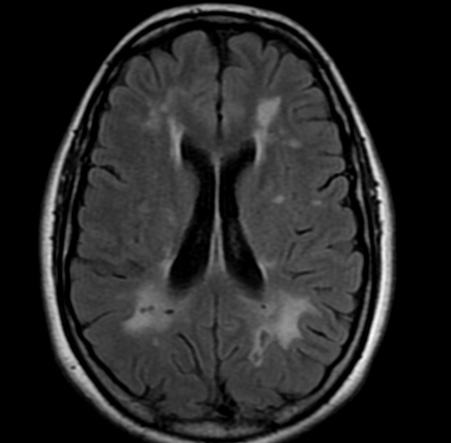
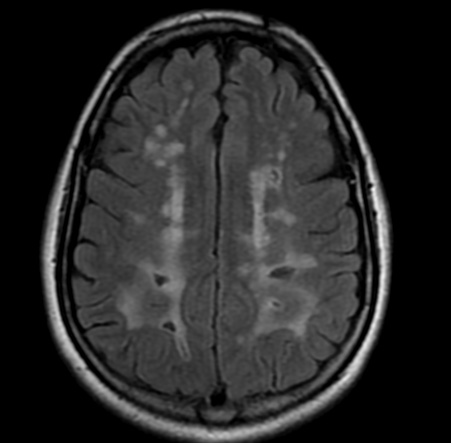
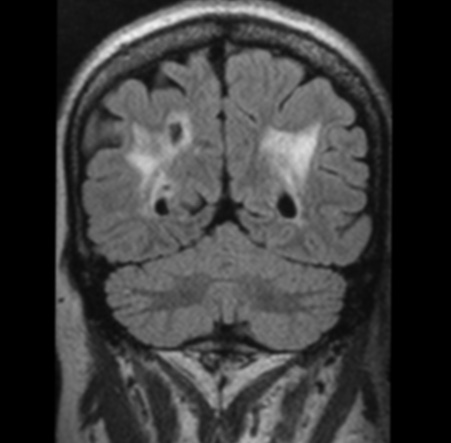
Patients with encephalopathy have memory loss, confusion, ataxia, incoordination, weakness, and upper motor neuron signs including increased muscle tone, deep tendon reflexes, and a positive Babinski reflex. Seizures, intracranial hemorrhages, dementia, and organic psychoses occur less frequently. Eosinophilic meningitis occurs uncommonly. The pathogenesis of both the encephalopathy and peripheral neuropathy of HES remains unknown. Possible mechanisms include direct damage from the infiltration of eosinophils and other inflammatory cells and injury from a toxin originating within eosinophils.
Embolic disease to the CNS may be caused by intracardiac thrombus formation secondary to eosinophilic infiltration resulting in endomyocardial fibrosis and thrombus formation. However, thromboemboli may also occur without demonstrable cardiac disease and can be the presenting manifestation of HES. In these cases, it has been postulated that thrombosis within the vessels of the CNS may be the underlying mechanism.
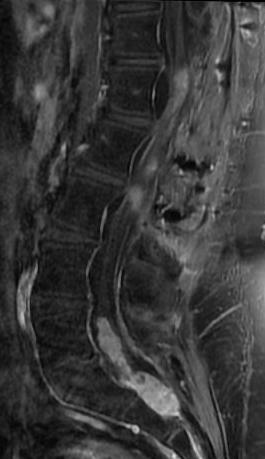
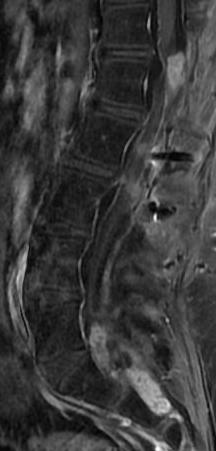
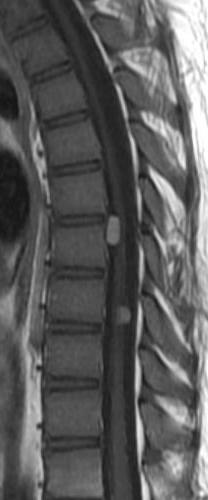
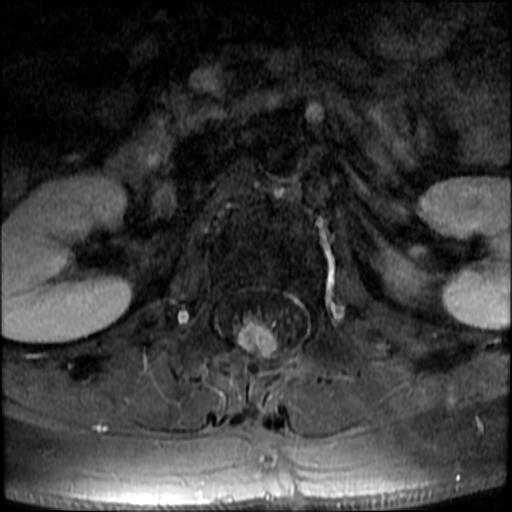
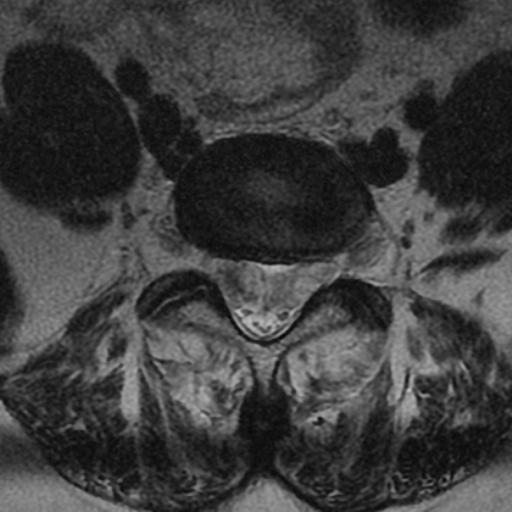
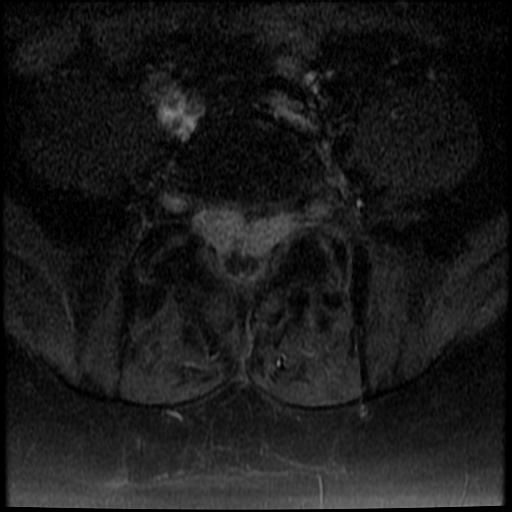
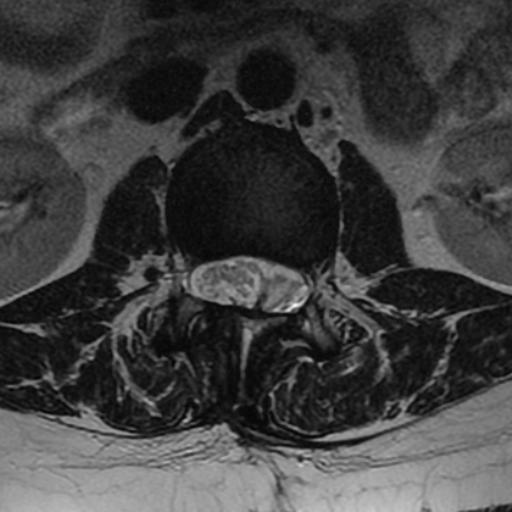
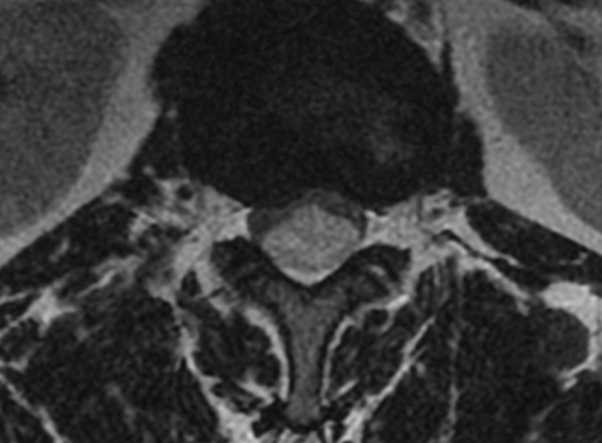
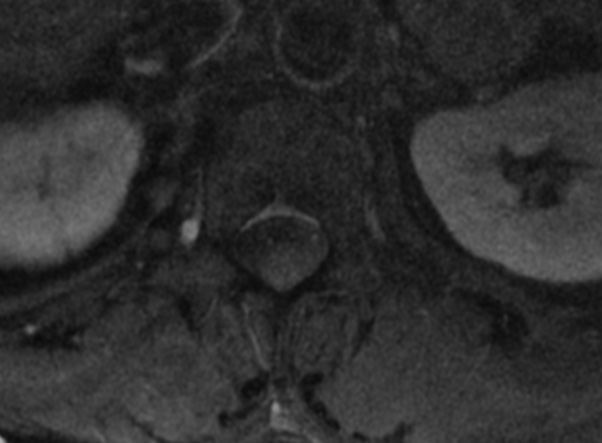
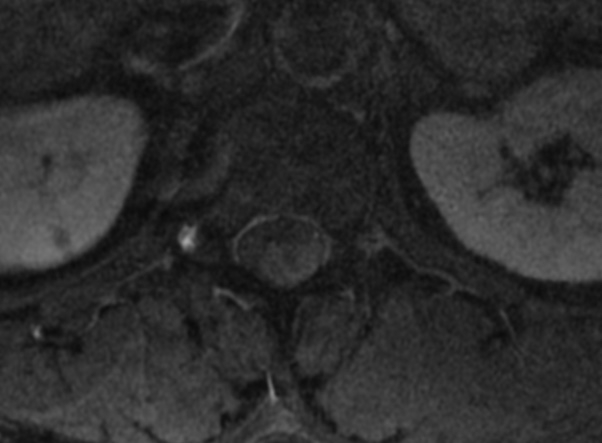
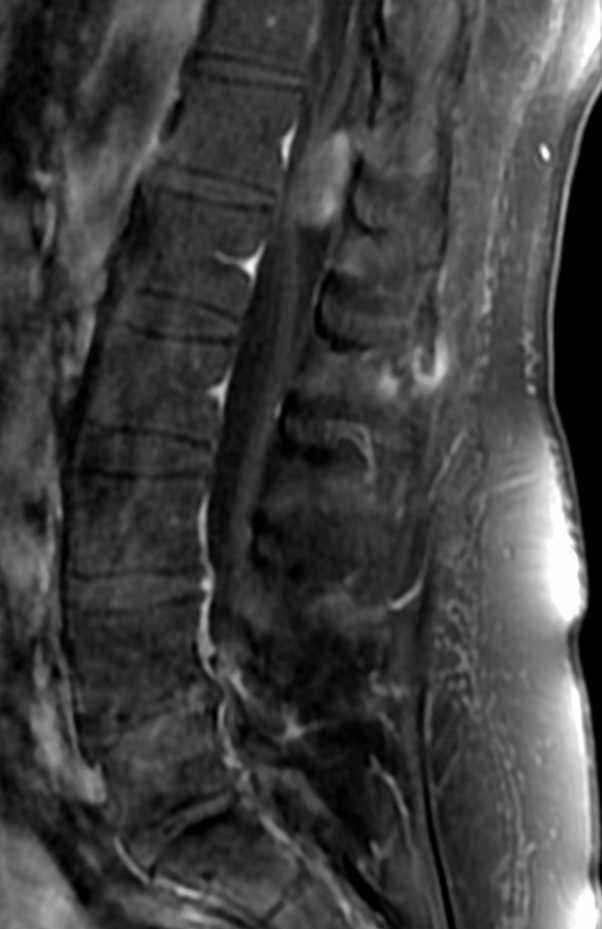
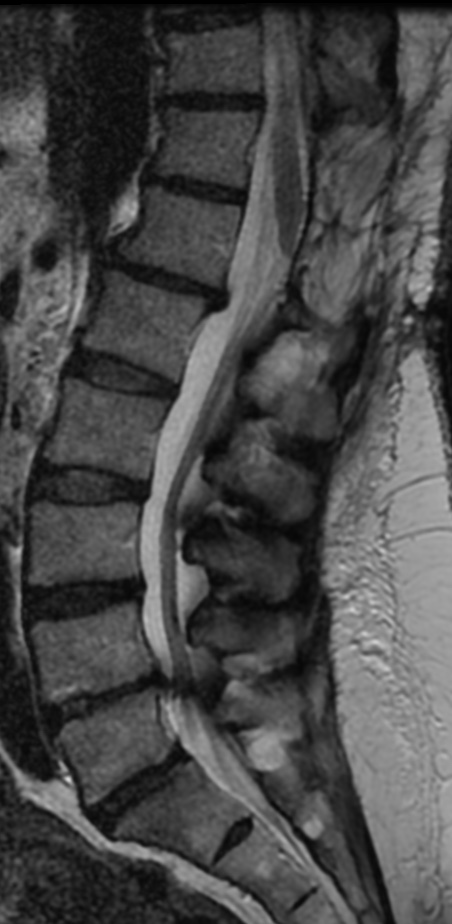
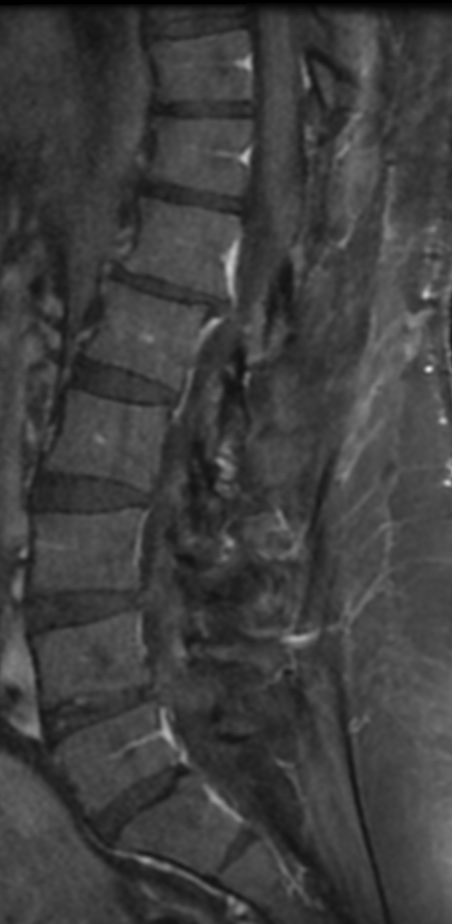
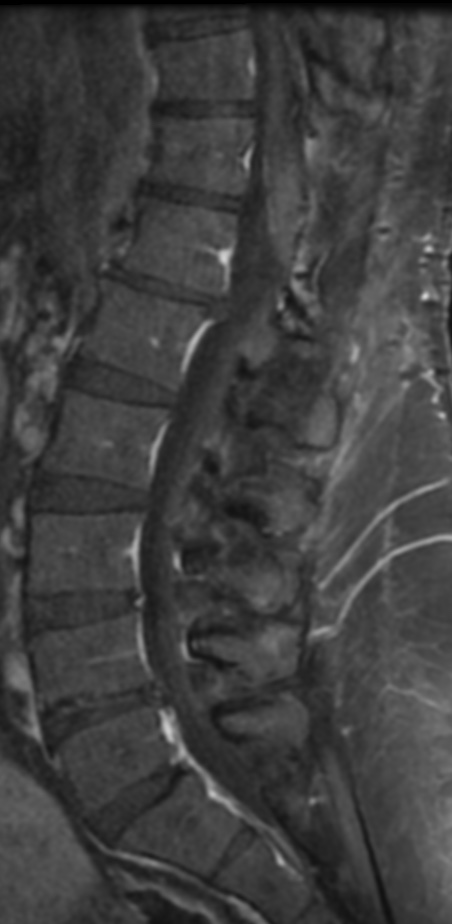
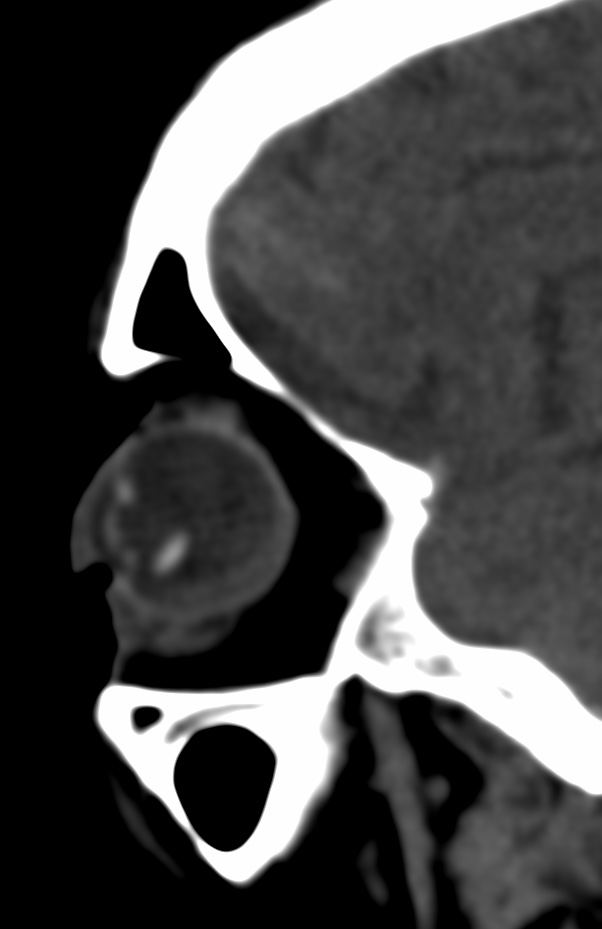
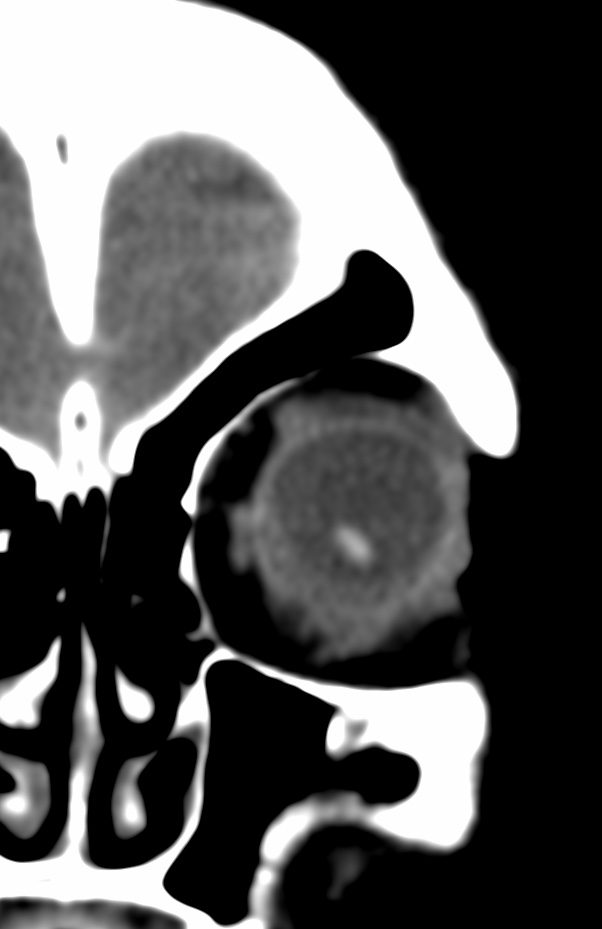
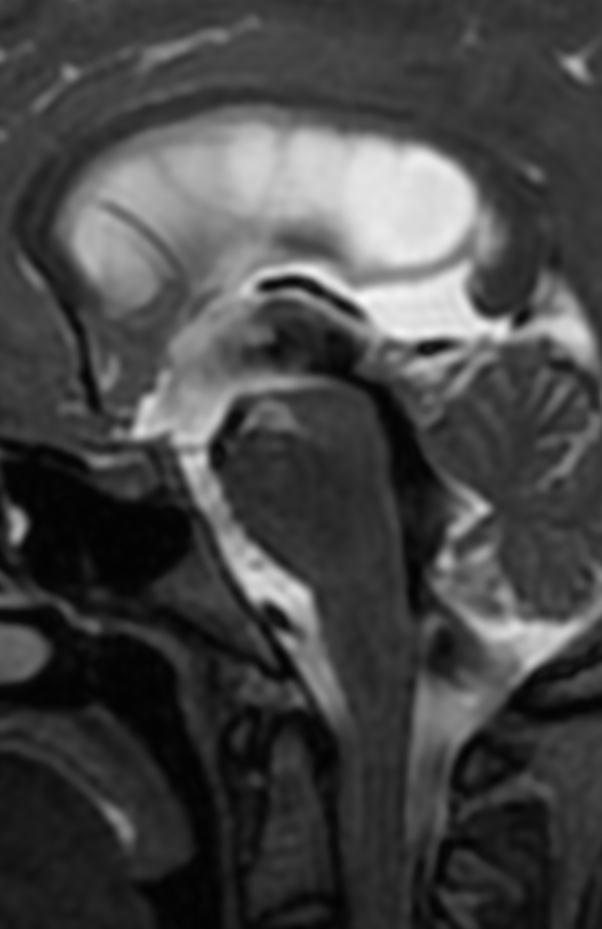
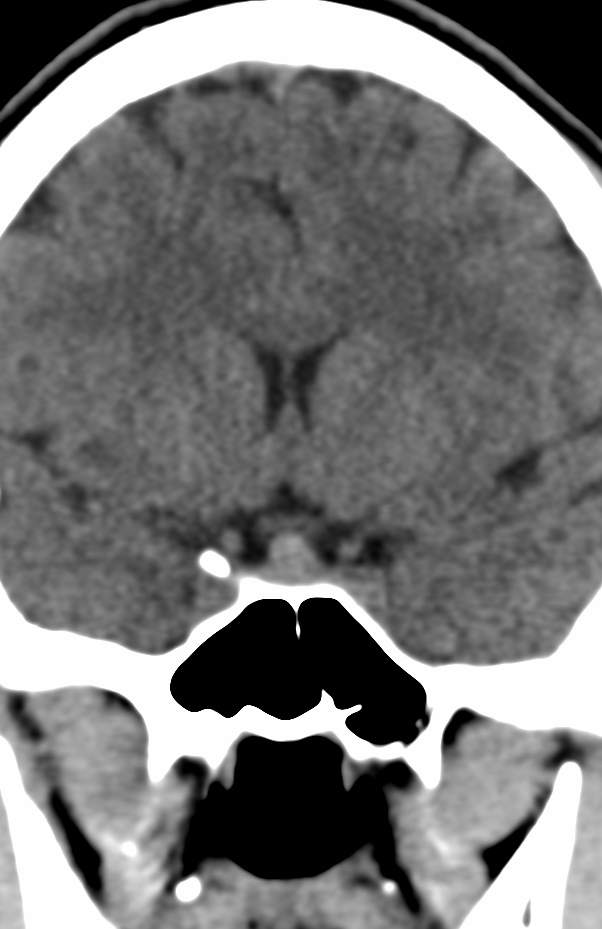
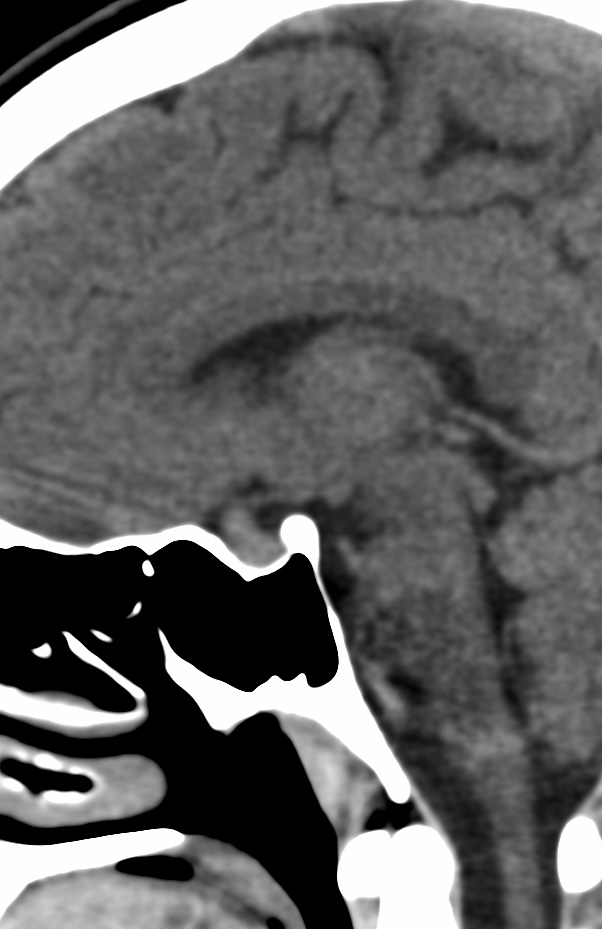
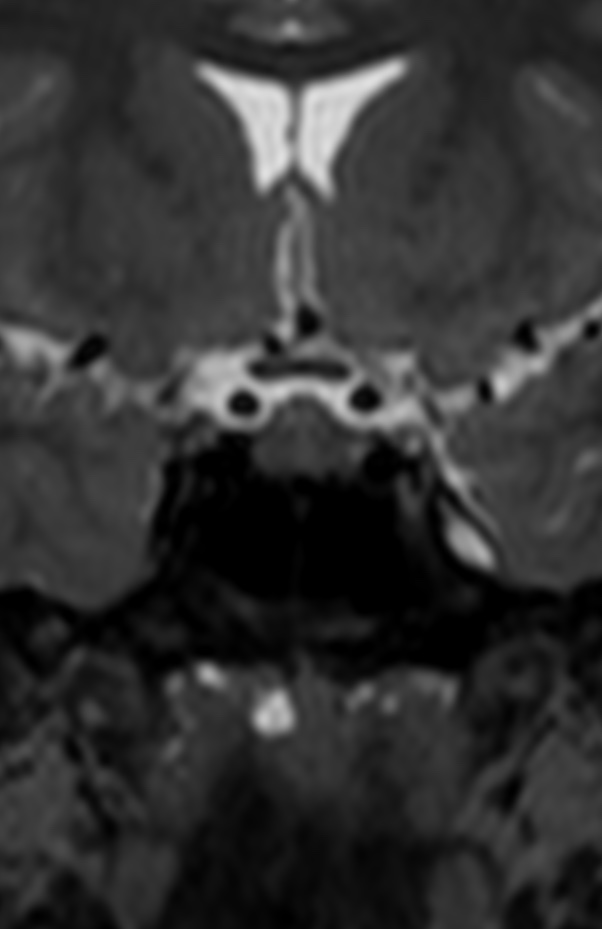
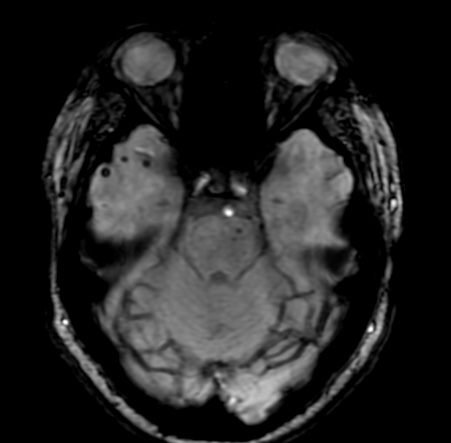
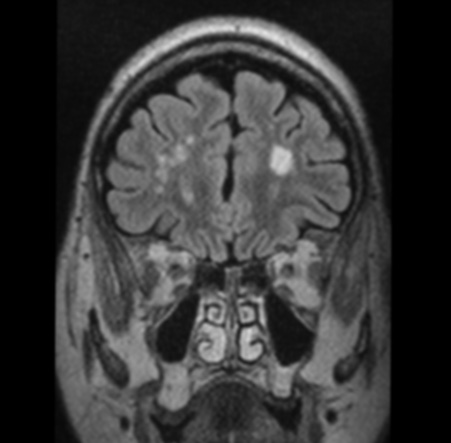
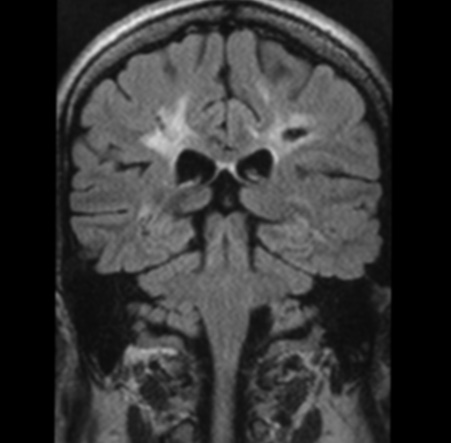
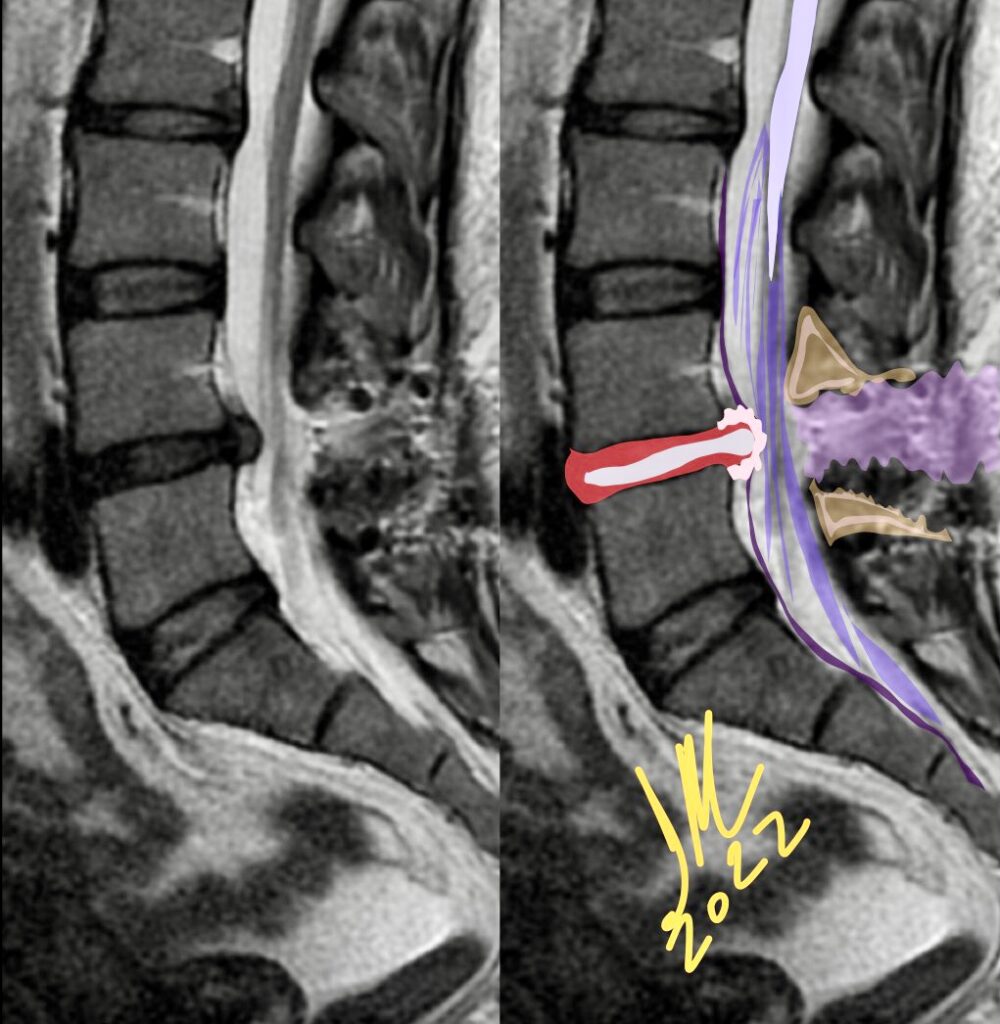
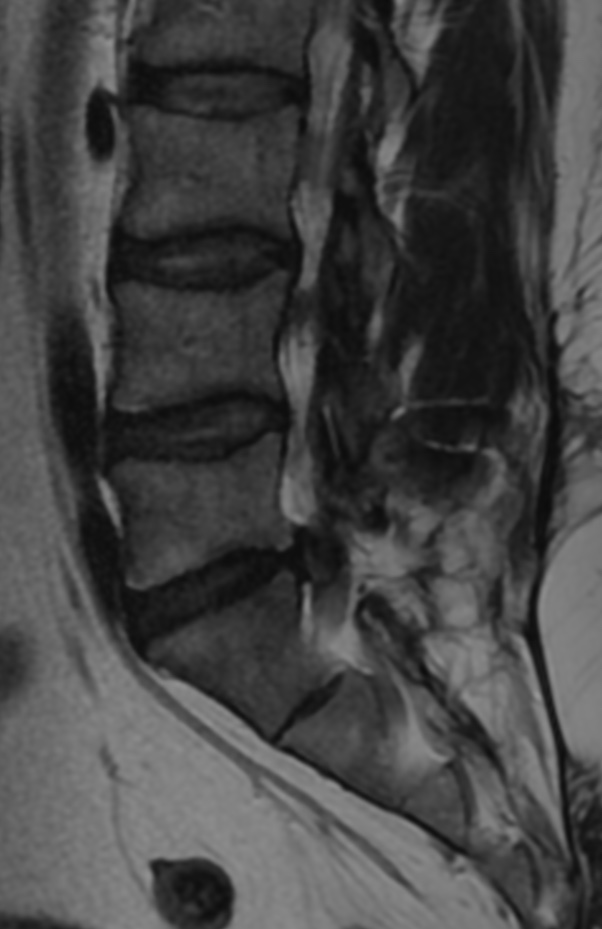
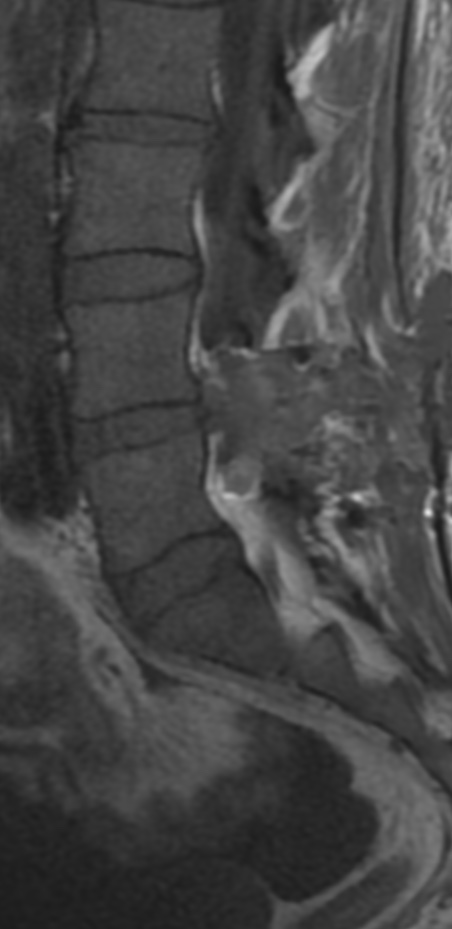
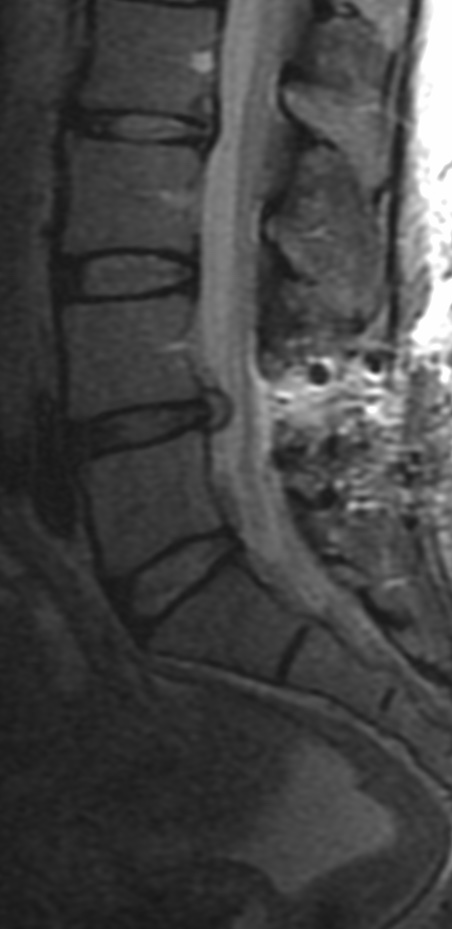
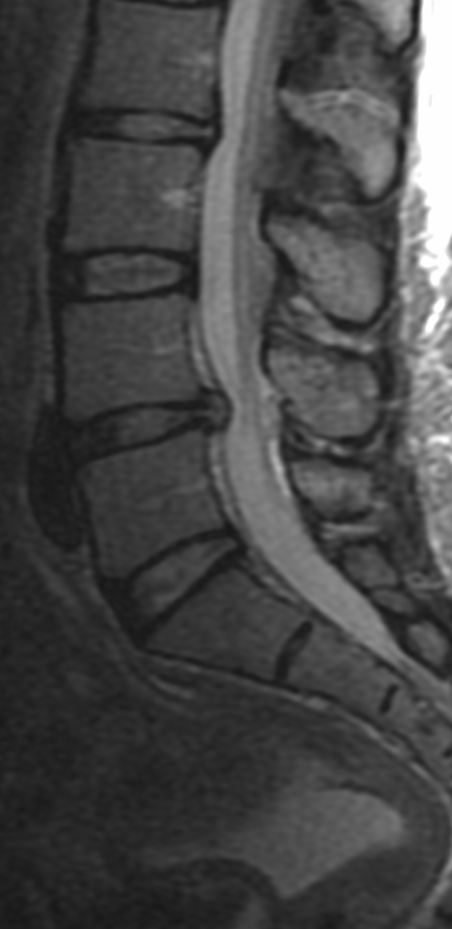
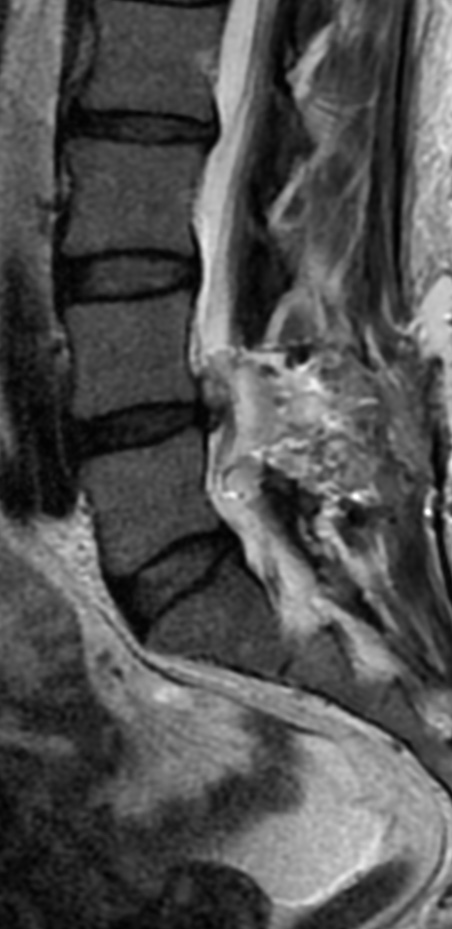
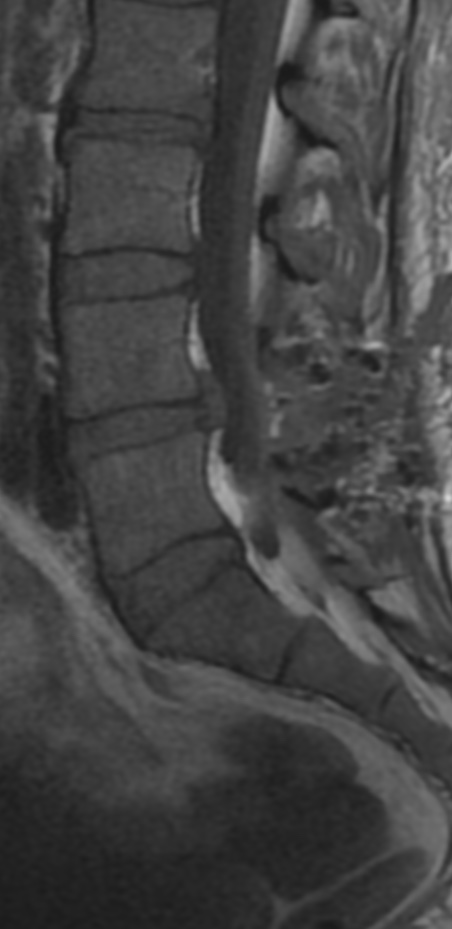
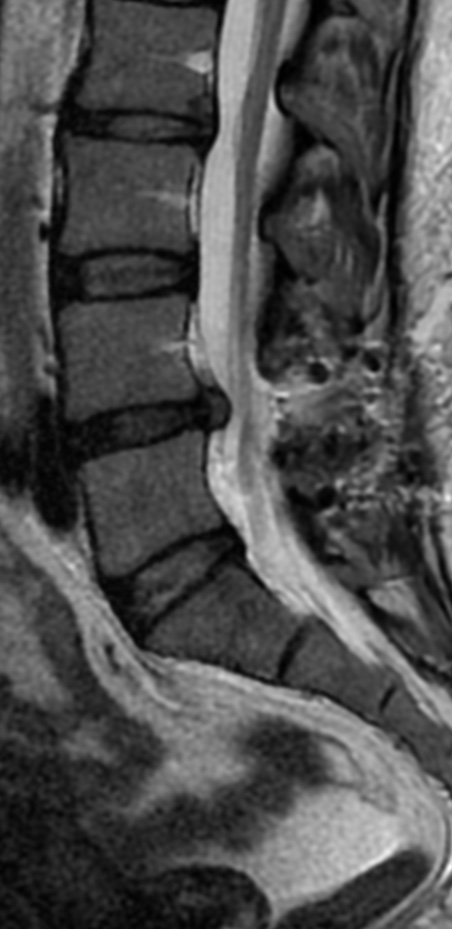
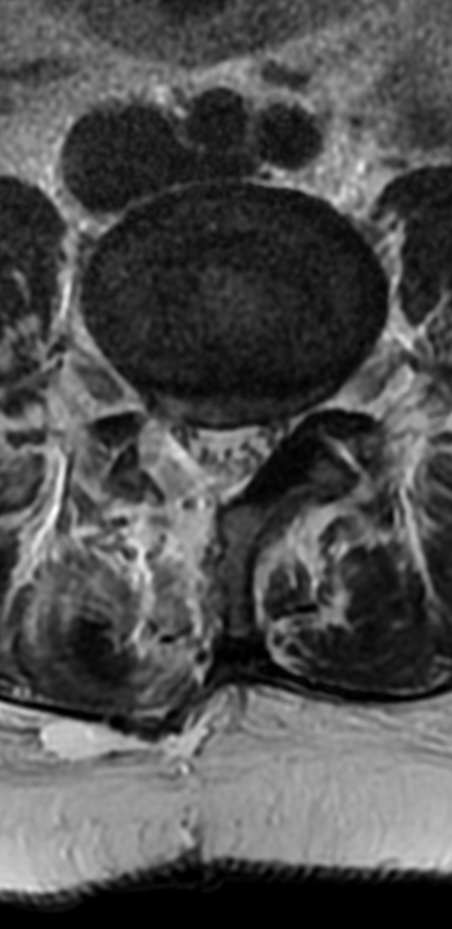
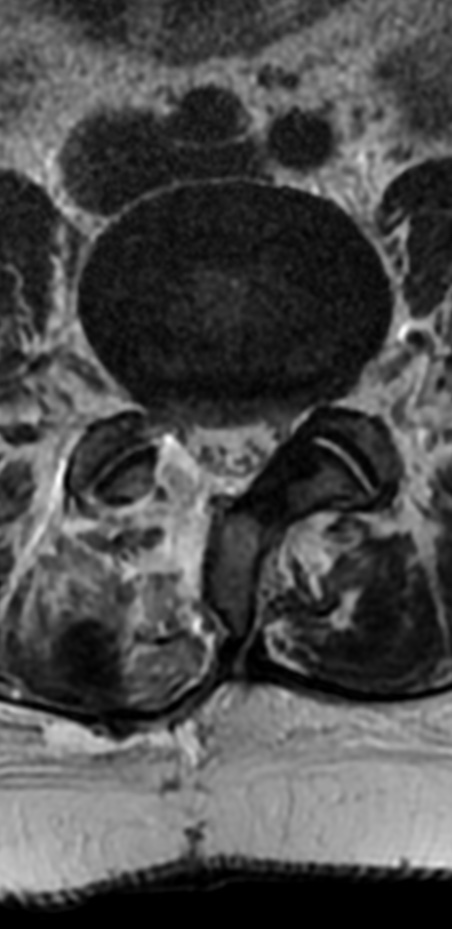
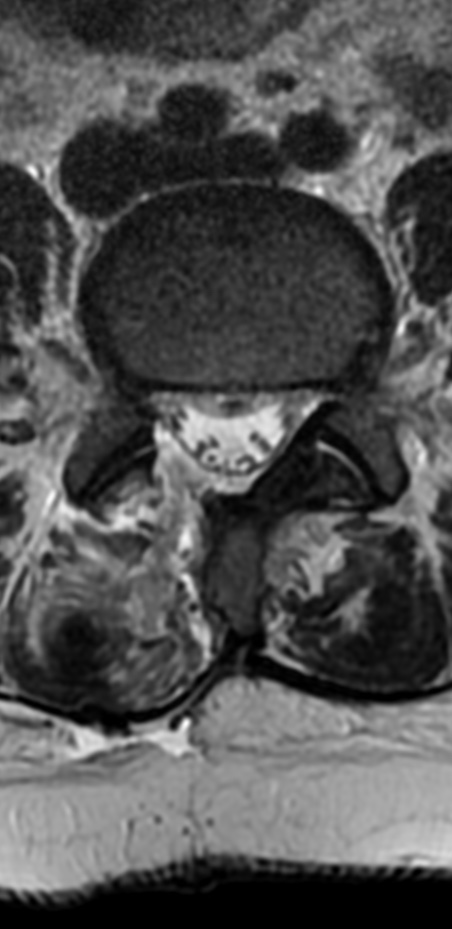
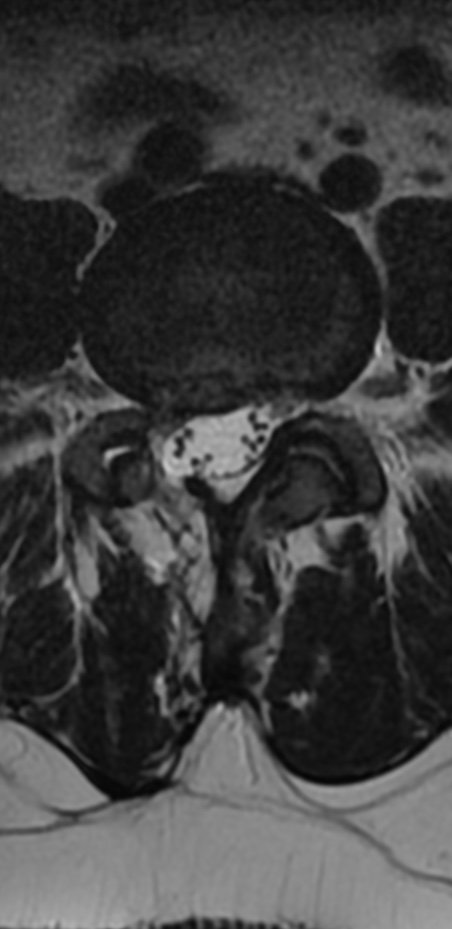
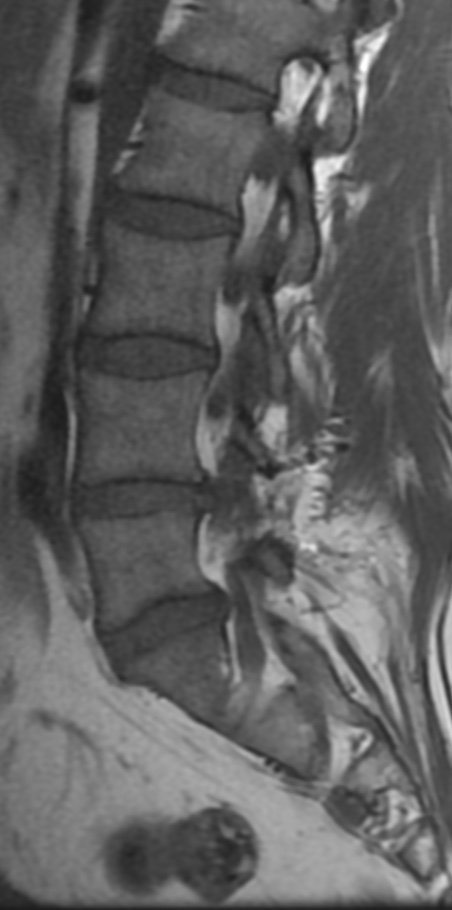
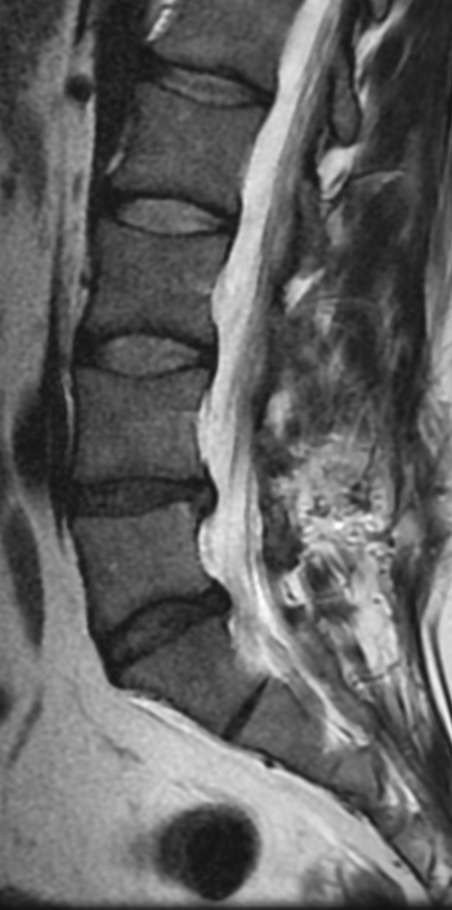
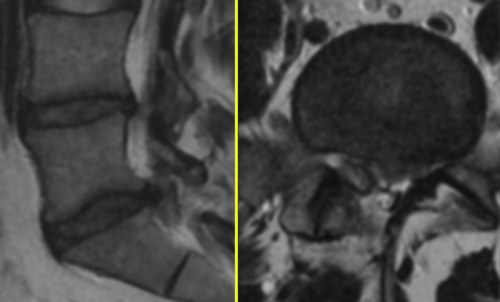
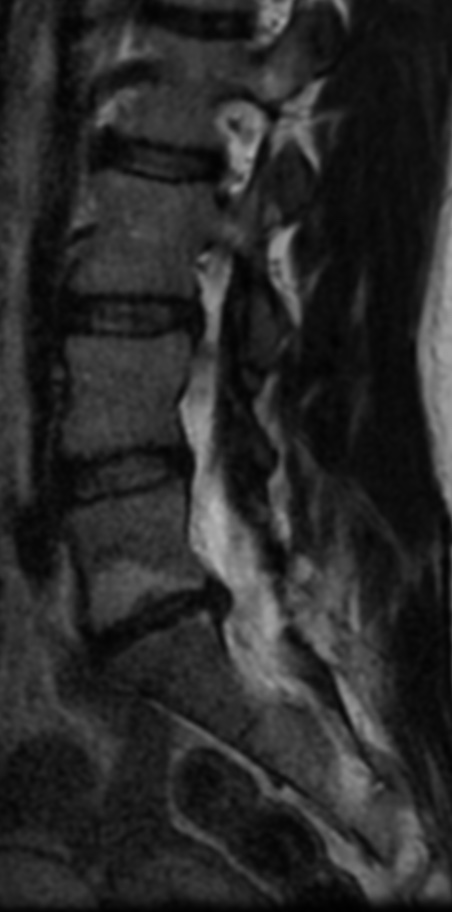
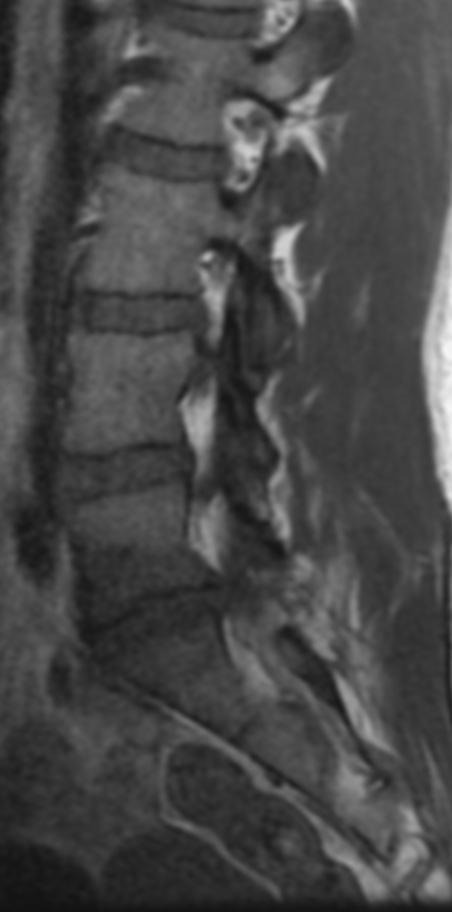
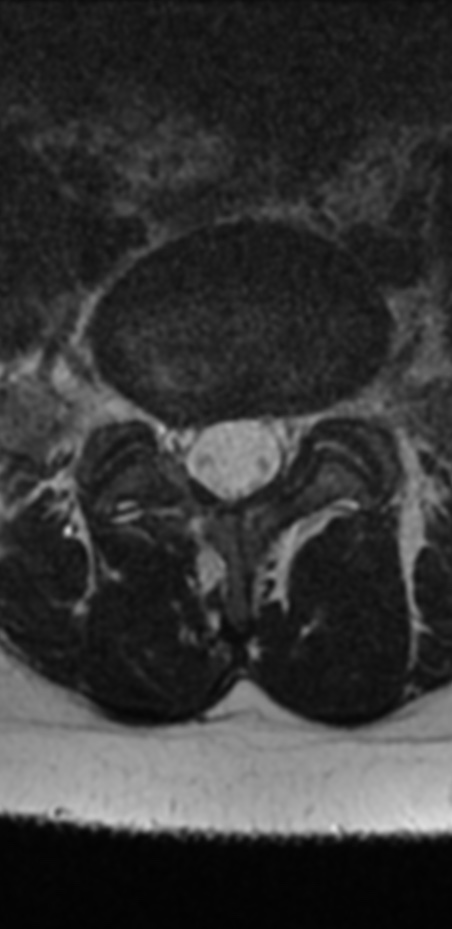
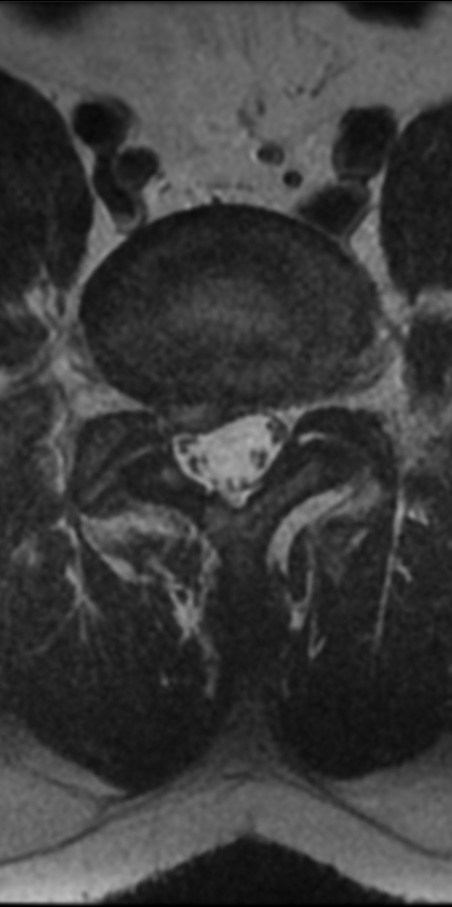
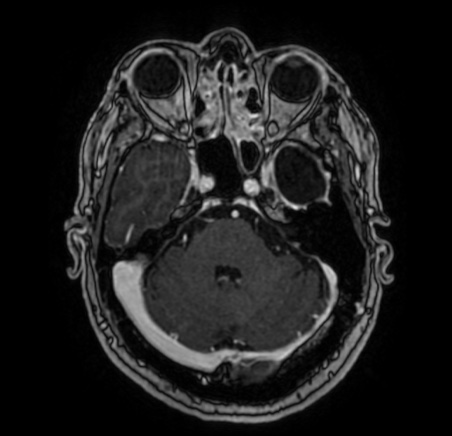
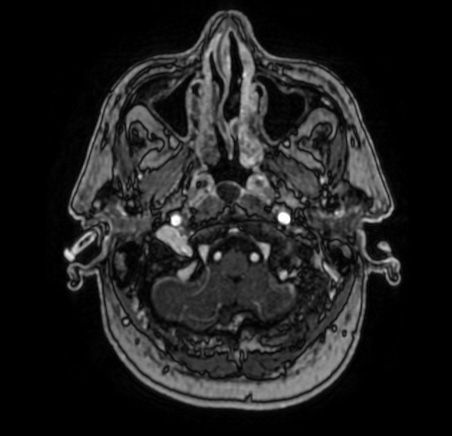
IPT is a clinicopathologic term used to describe a reactive inflammatory and nonneoplastic process. In the literature, “pseudotumor” has been given many different names, some of which are plasma cell granuloma, plasmacytoma, inflammatory myofibroblastic tumor proliferation, and histiocytoma. IPT has been described most often in the lung and orbit, with other systemic sites somewhat less frequently. Involvement of the CNS parenchyma by IPT is rare. The lesions occur throughout the brain parenchyma and meninges, without restriction to a particular area. IPT can both clinically and radiologically mimic a malignant process.
The differential diagnostic considerations of a mass in the cavernous sinus with dural enhancement include meningioma, lymphoma, neurosarcoidosis, infection, and amyloidosis.
Reference:
American Journal of Neuroradiology May 2007, 28 (5) 971-973;