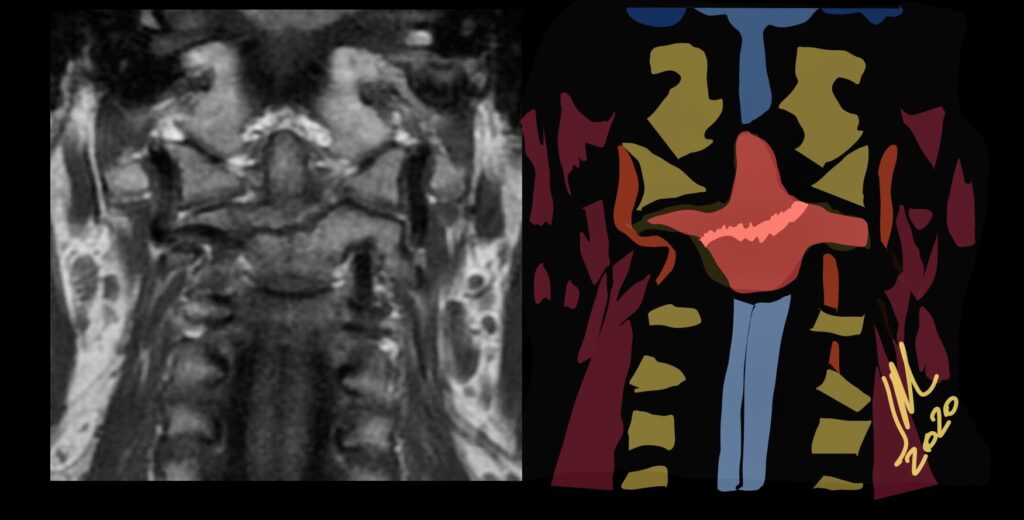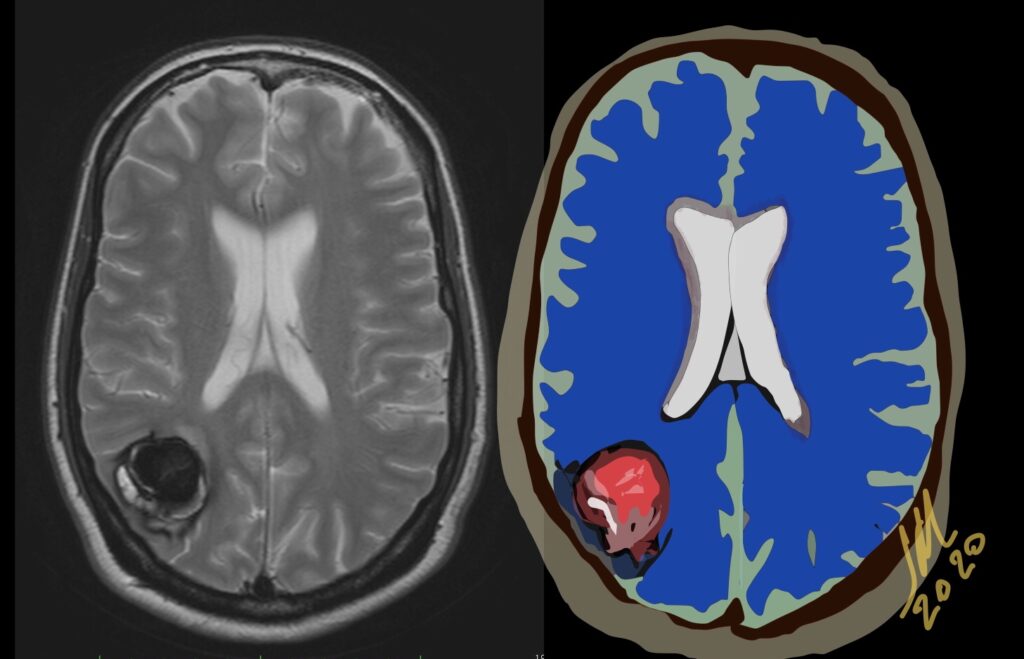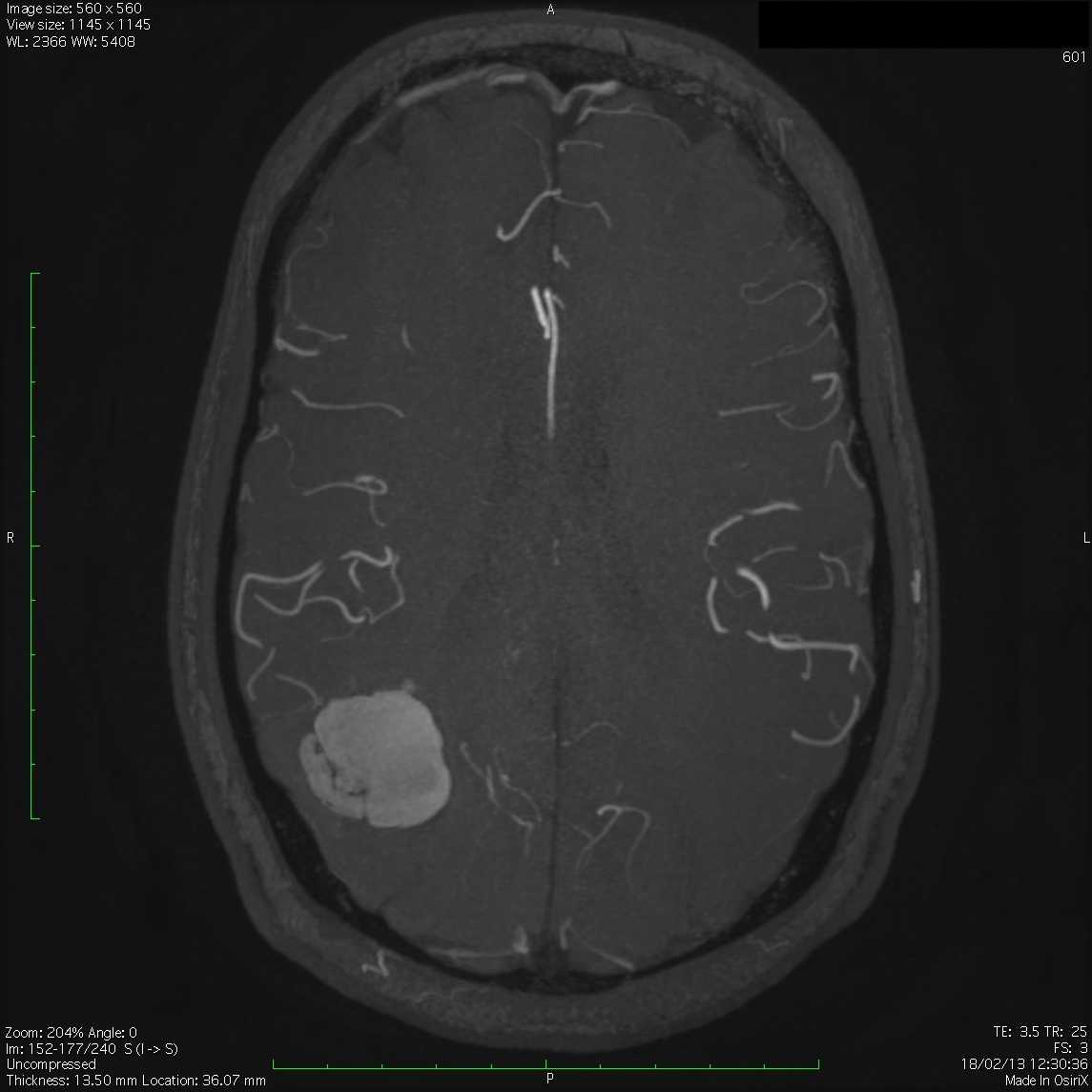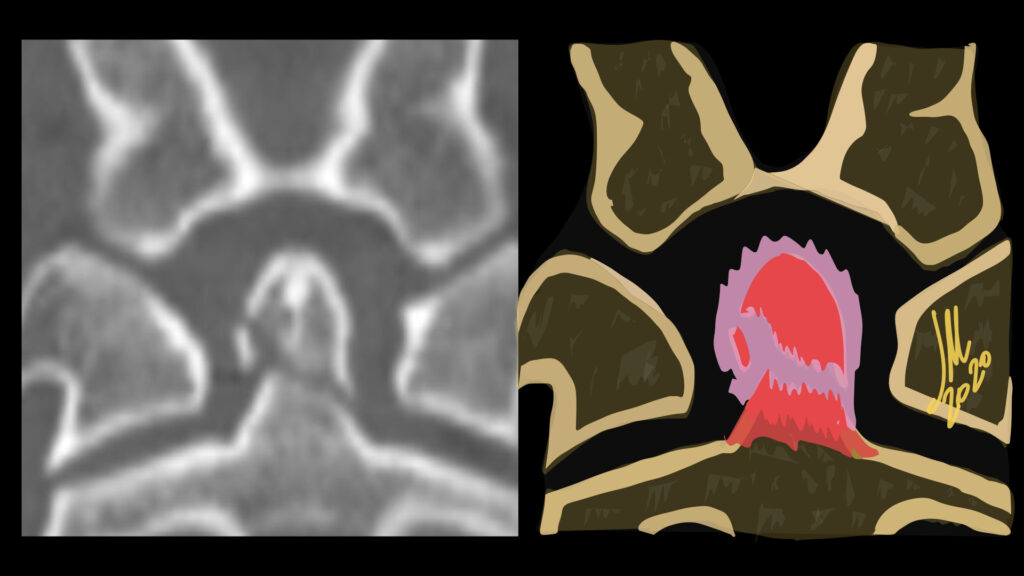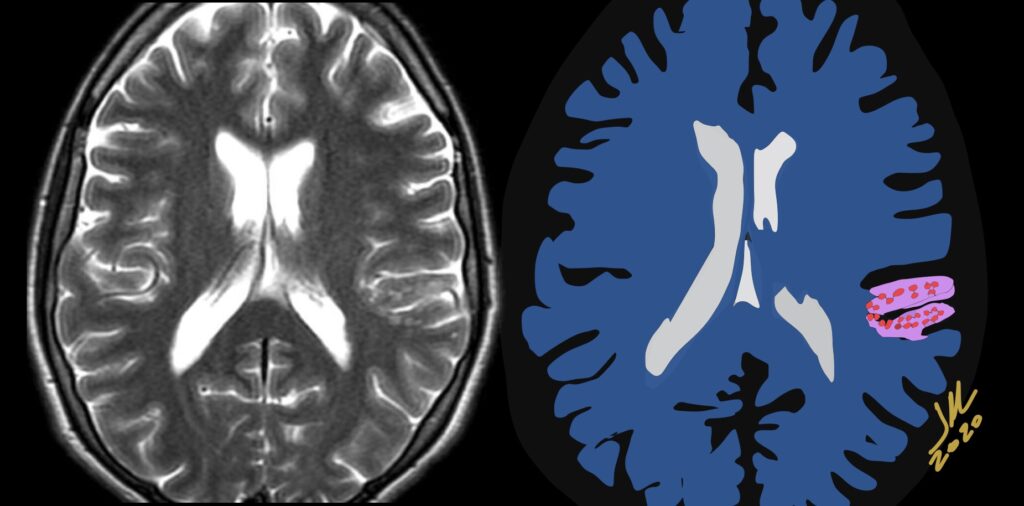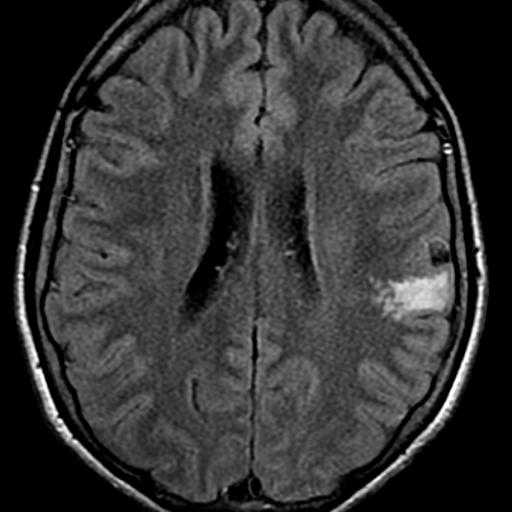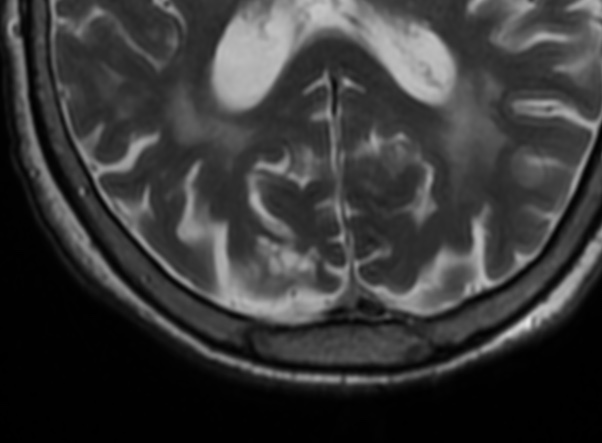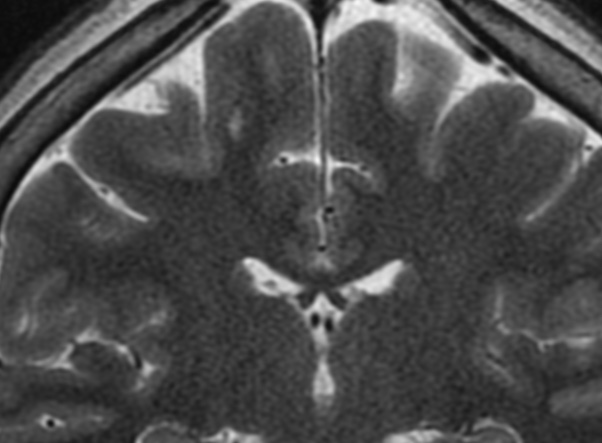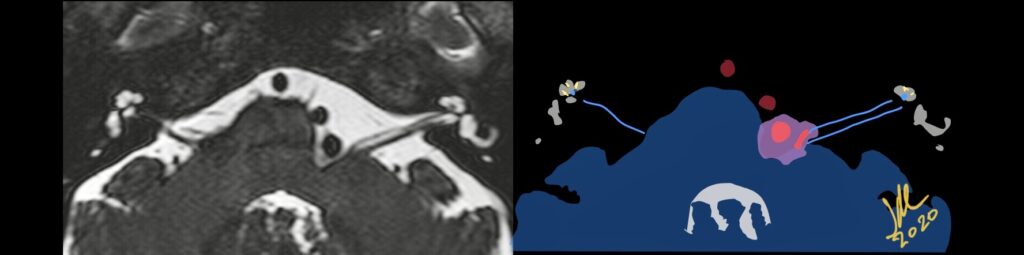
Neurovascular compression syndrome (NVCS) is defined as a direct contact with mechanical irritation of cranial nerves by blood vessels. By far the cases of neurovascular contact are clinically asymptomatic
NVCS can occur either at the root entry-exit zone 10%–90%, adjacent cisternal segment 60%, Transitional zone 22%.
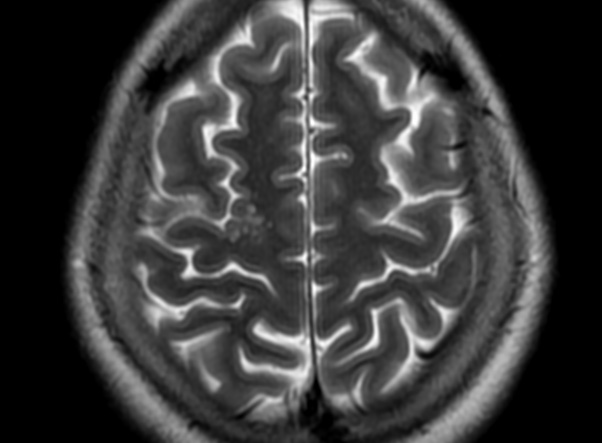
Microvascular decompression is highly effective in HFS and symptoms disappear after an operation in 90%–95% of cases; however, recurrence is seen in up to 25% of patients.
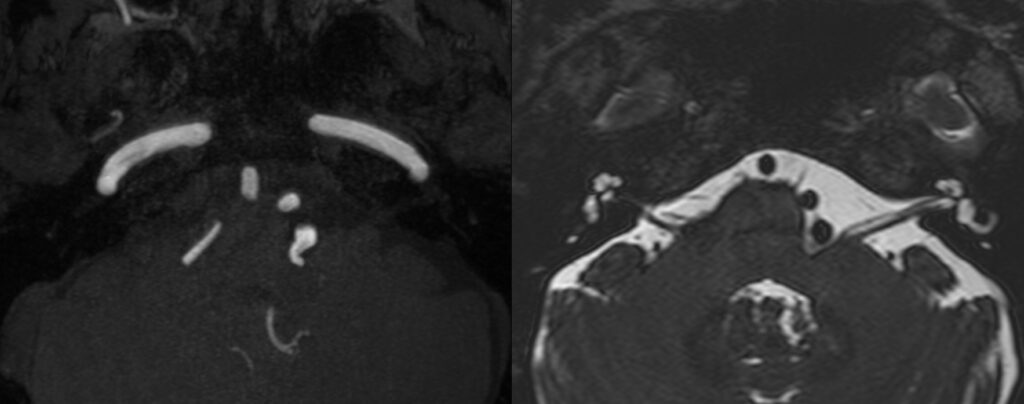
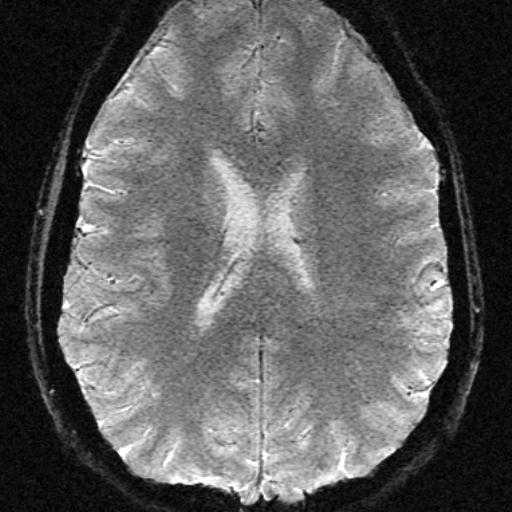
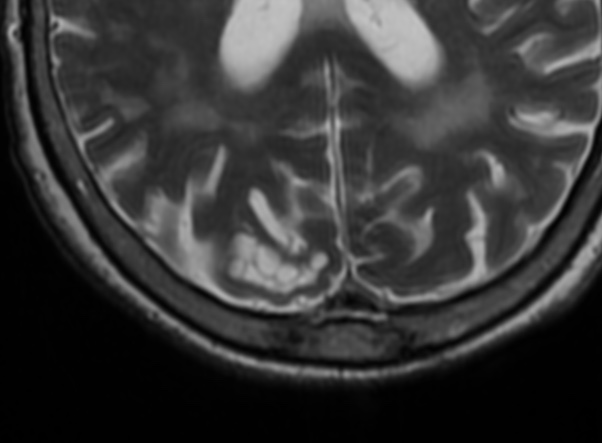
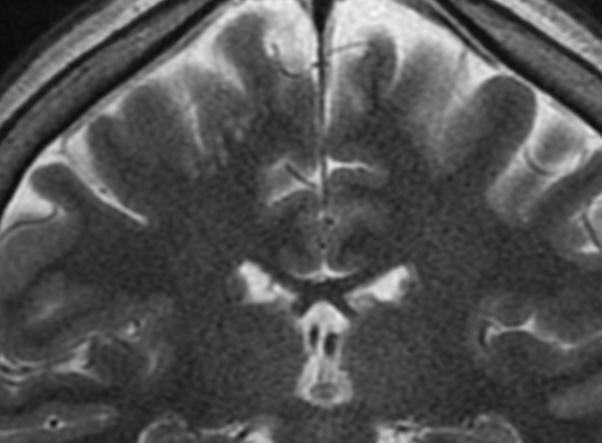
The transition zone between central and peripheral myelin is an anatomic area with increased mechanical vulnerability, which is of particular interest in the context of symptomatic NVCS. The transitional zone look to be the more relevant and vulnerable anatomic structure, and it is not always located in the same position as the root entrance-exit zone (TZ). Exact anatomic knowledge of the position and morphology of the TZ is of fundamental importance for the interpretation of neuroimaging findings in suspected NVCS. TZ of VII CN to be about <1mm to REZ.
To remember TZ location from REZ:
CN V = 2mm. CN VIII = 1mm. CN VIII= 10mm. CN IX= 15mm