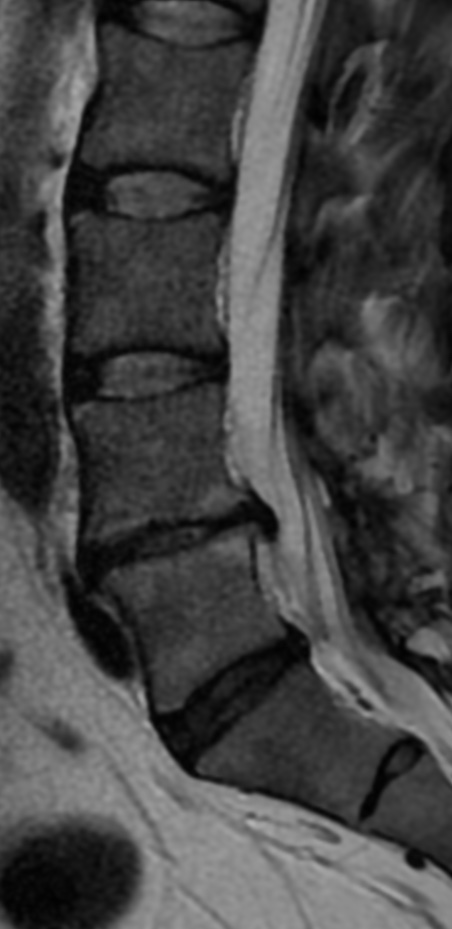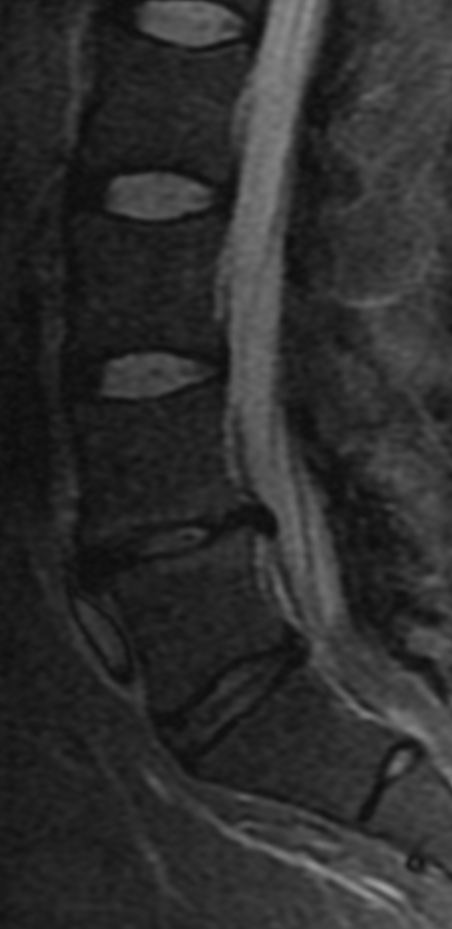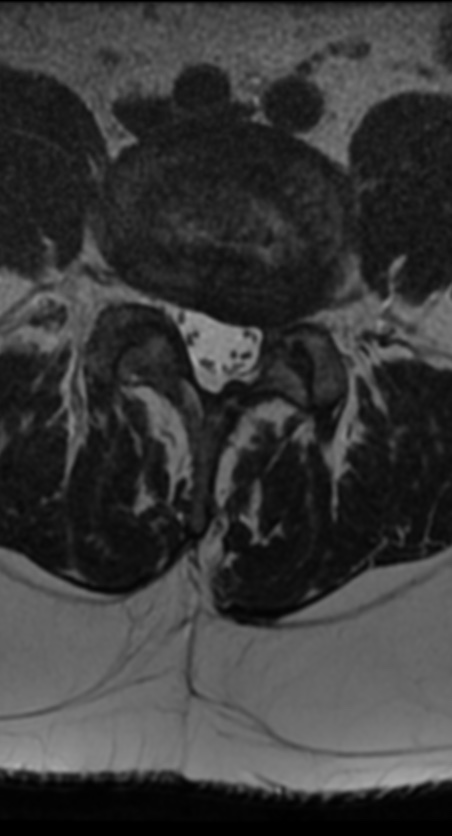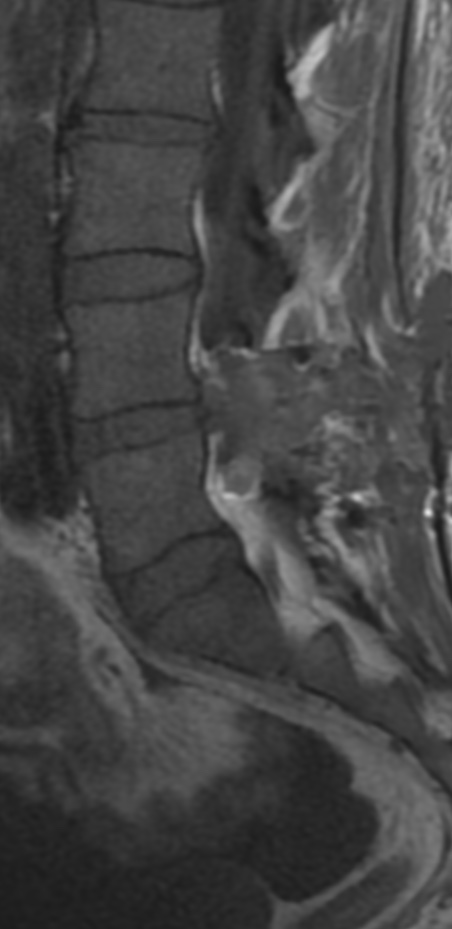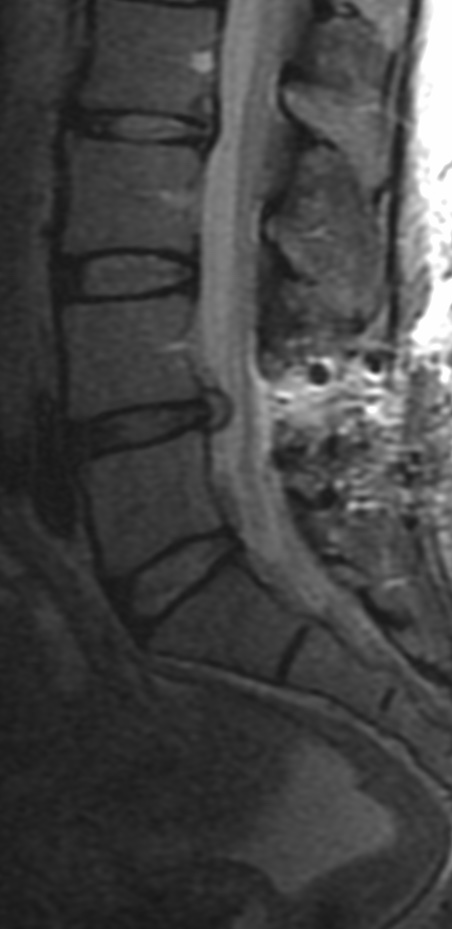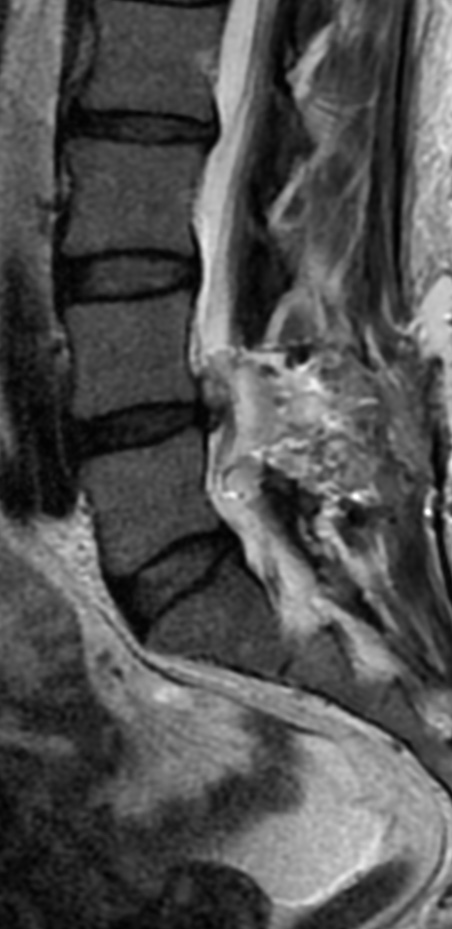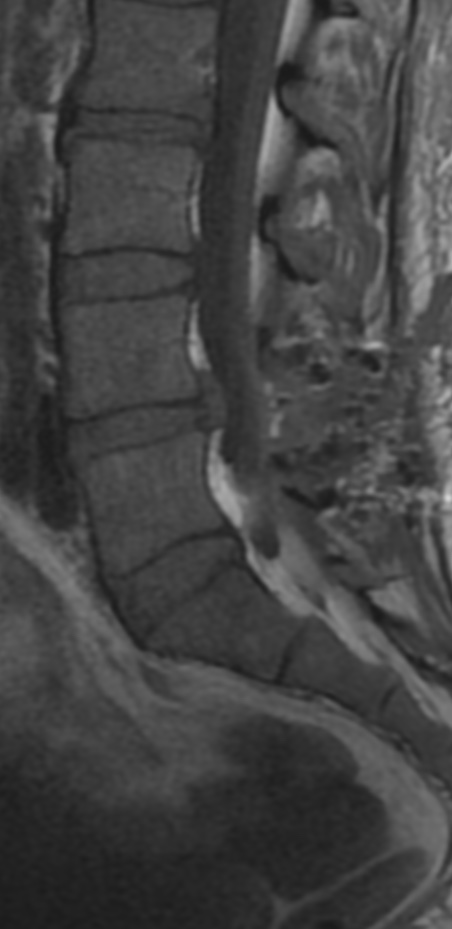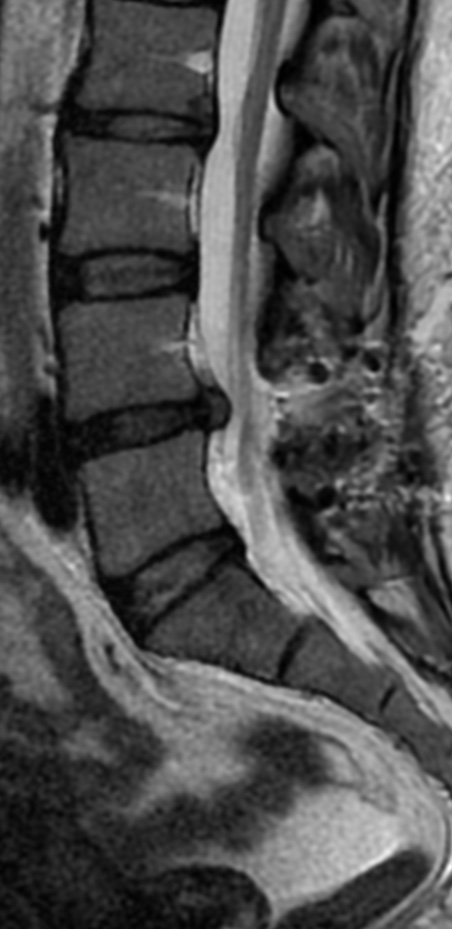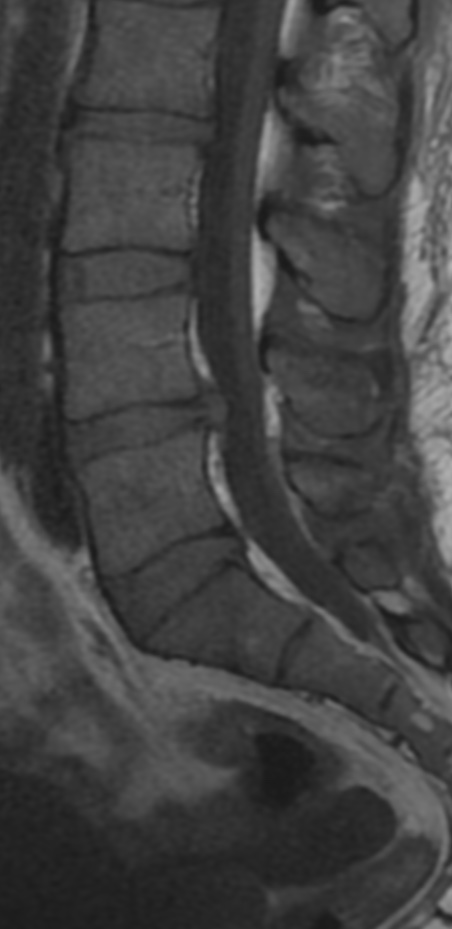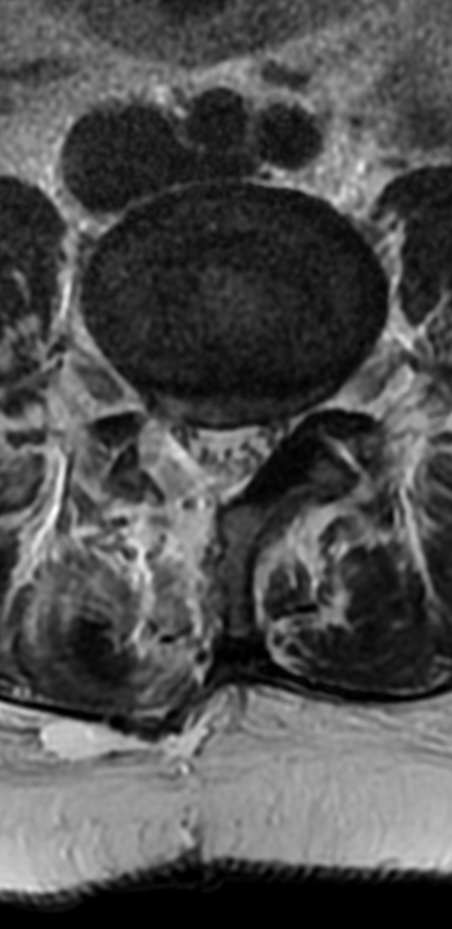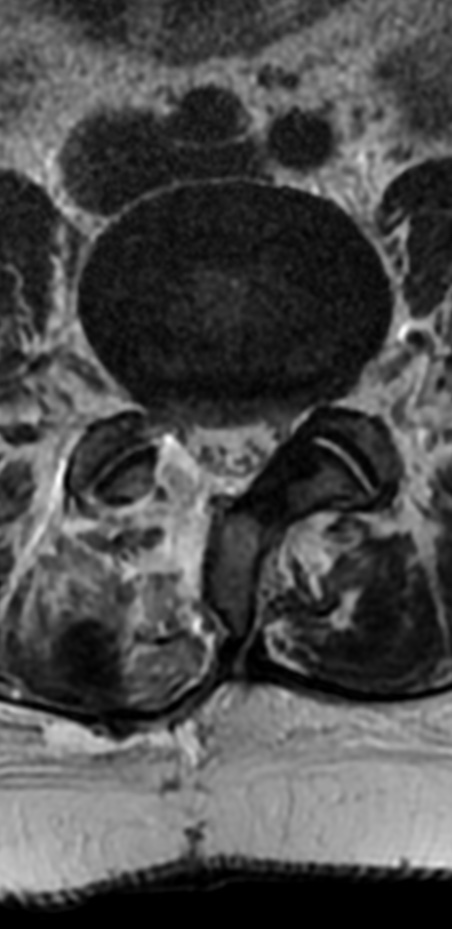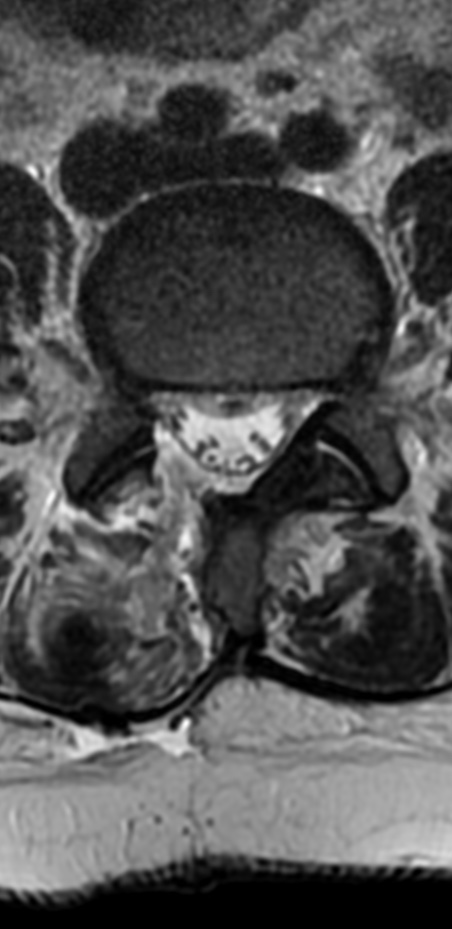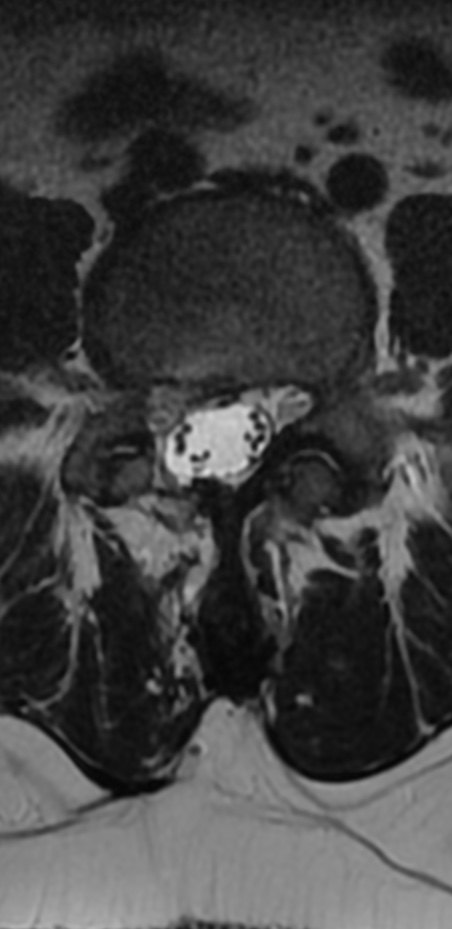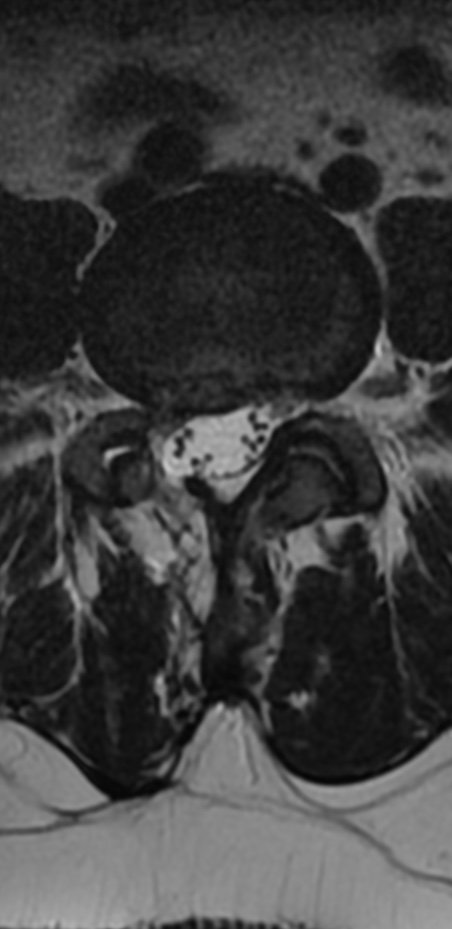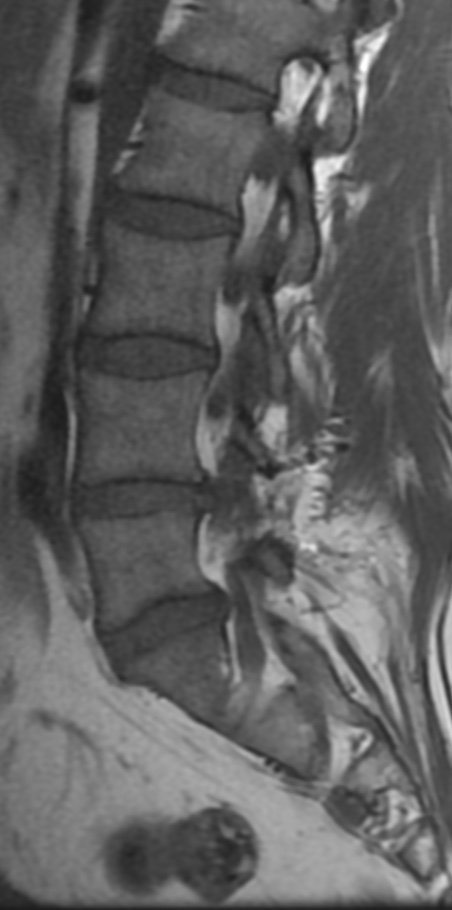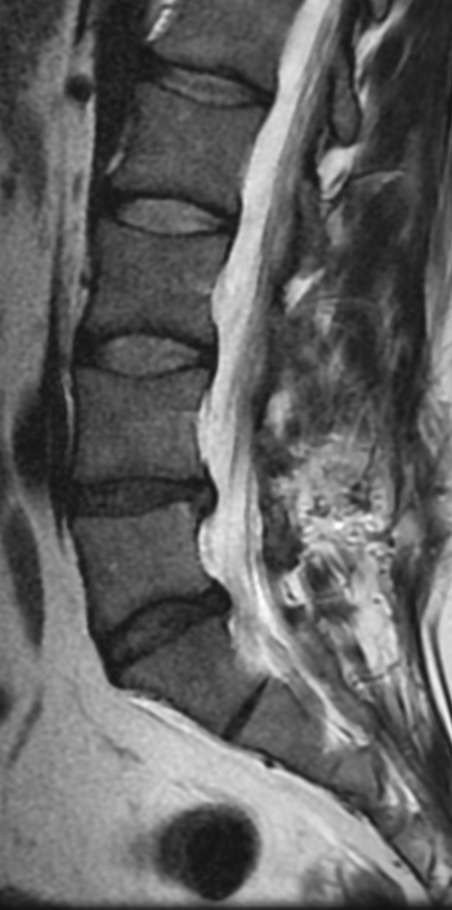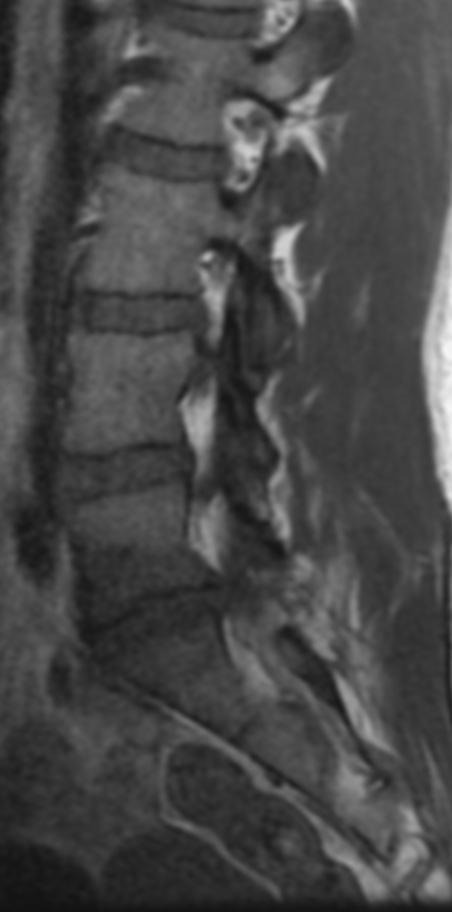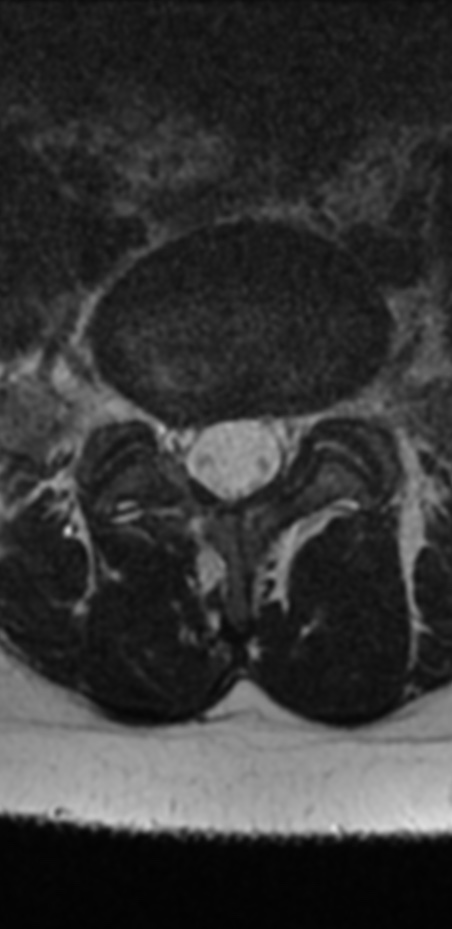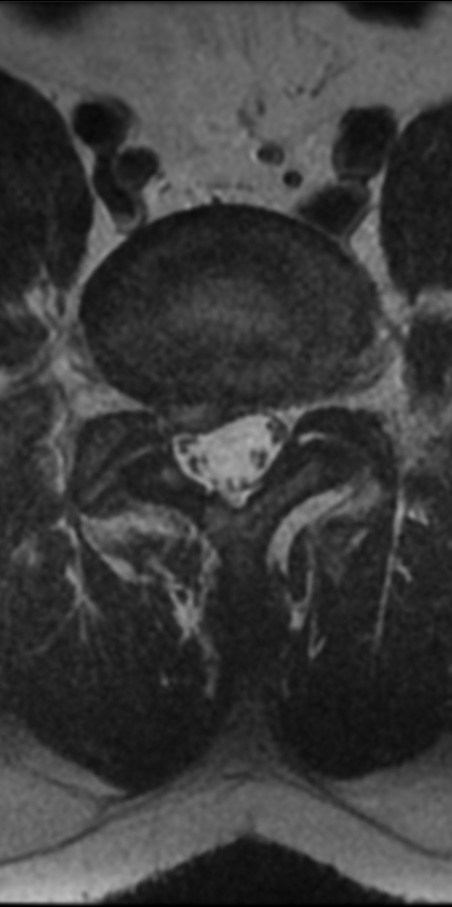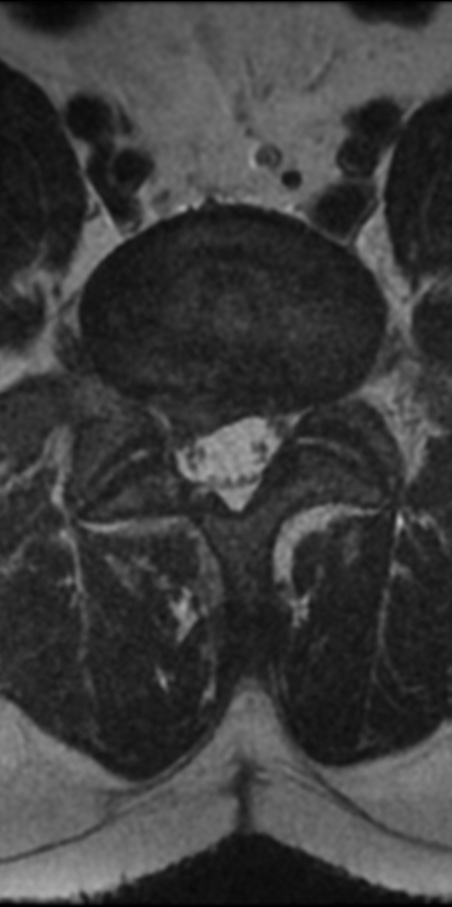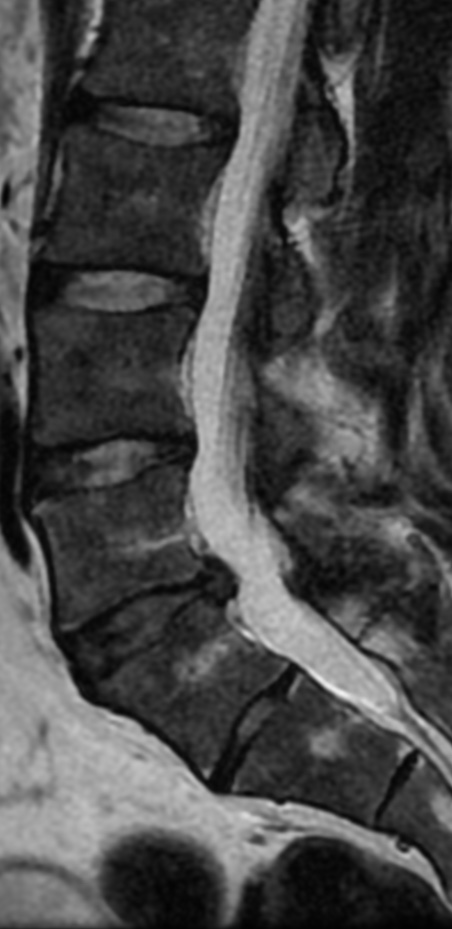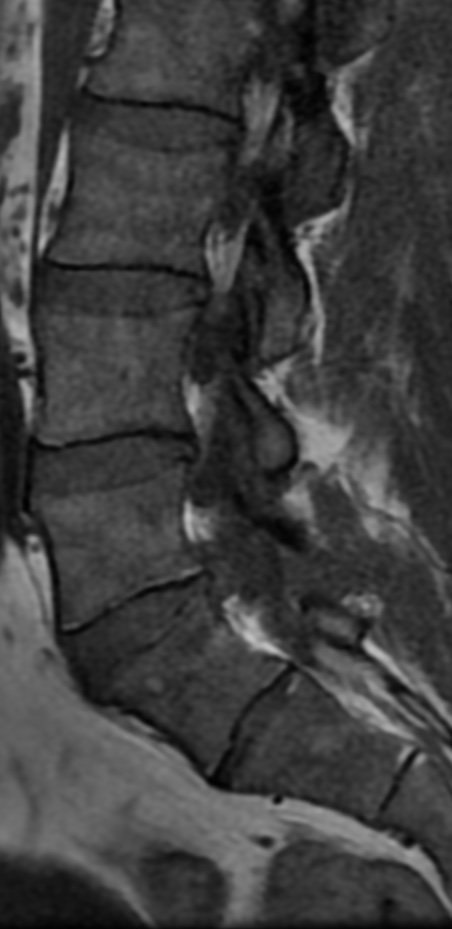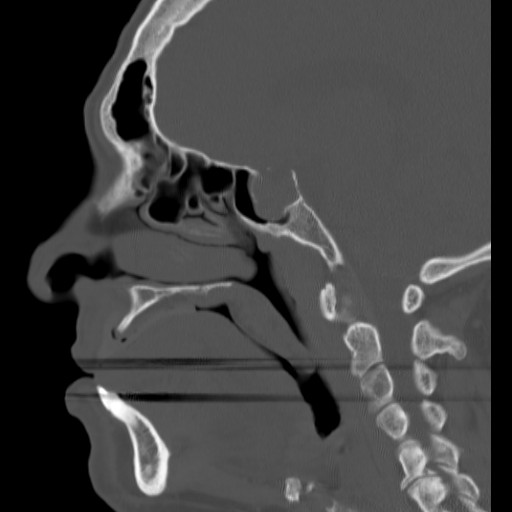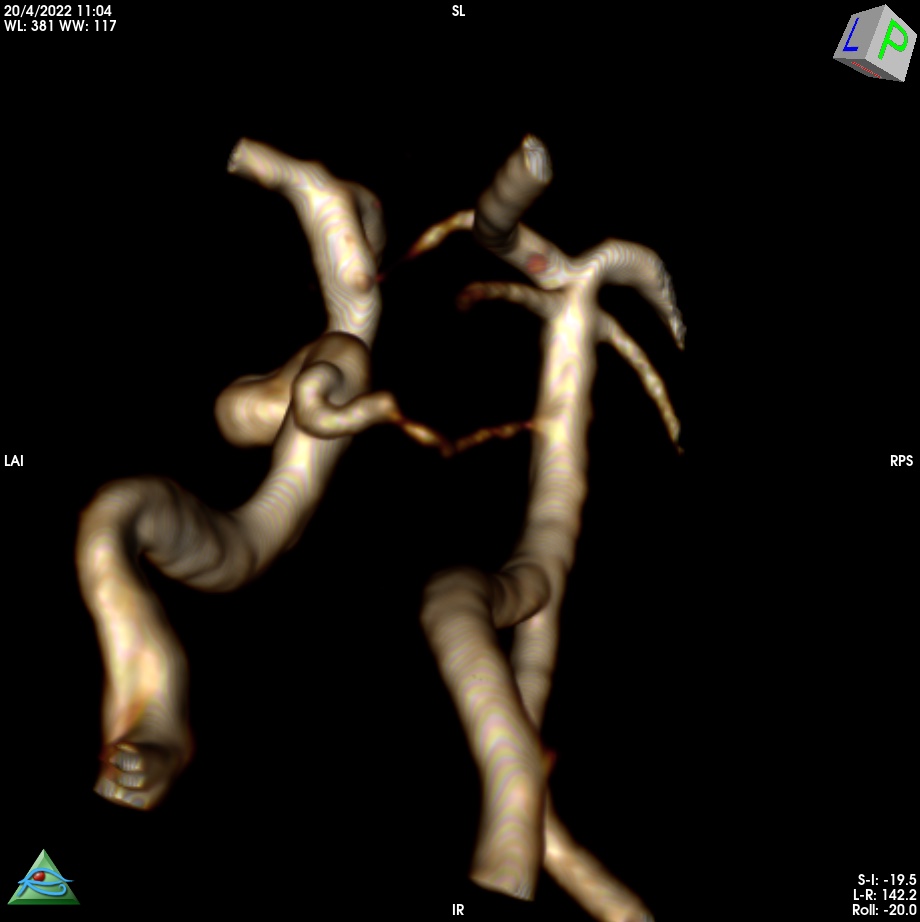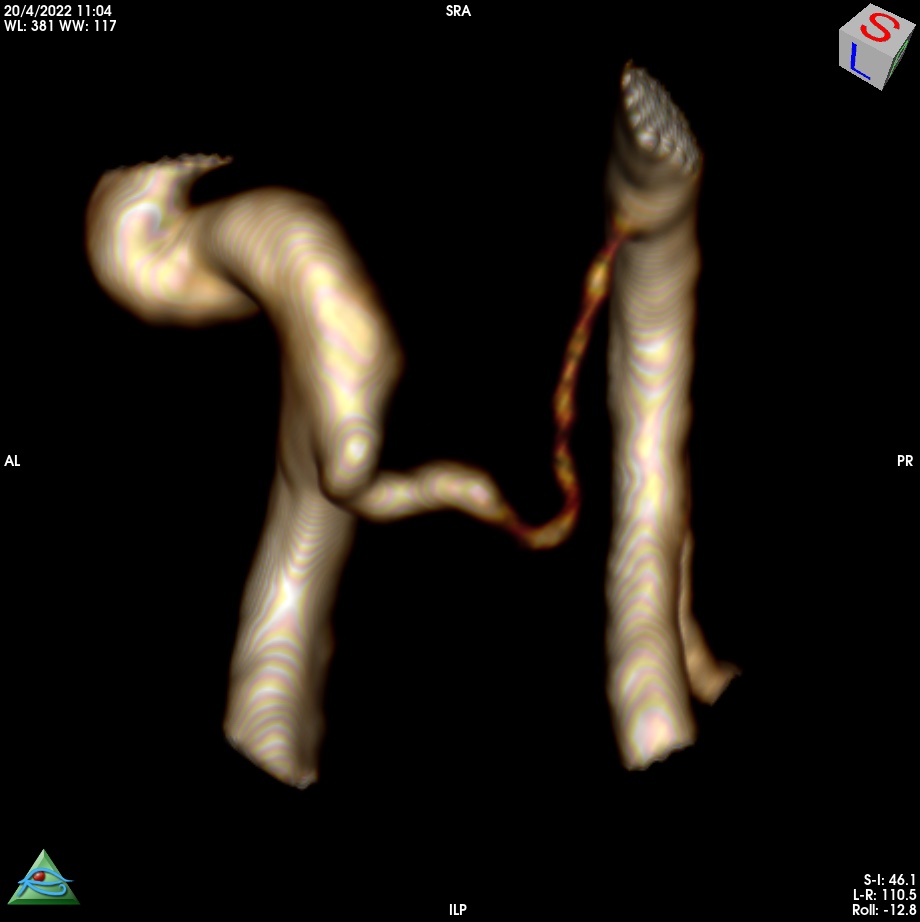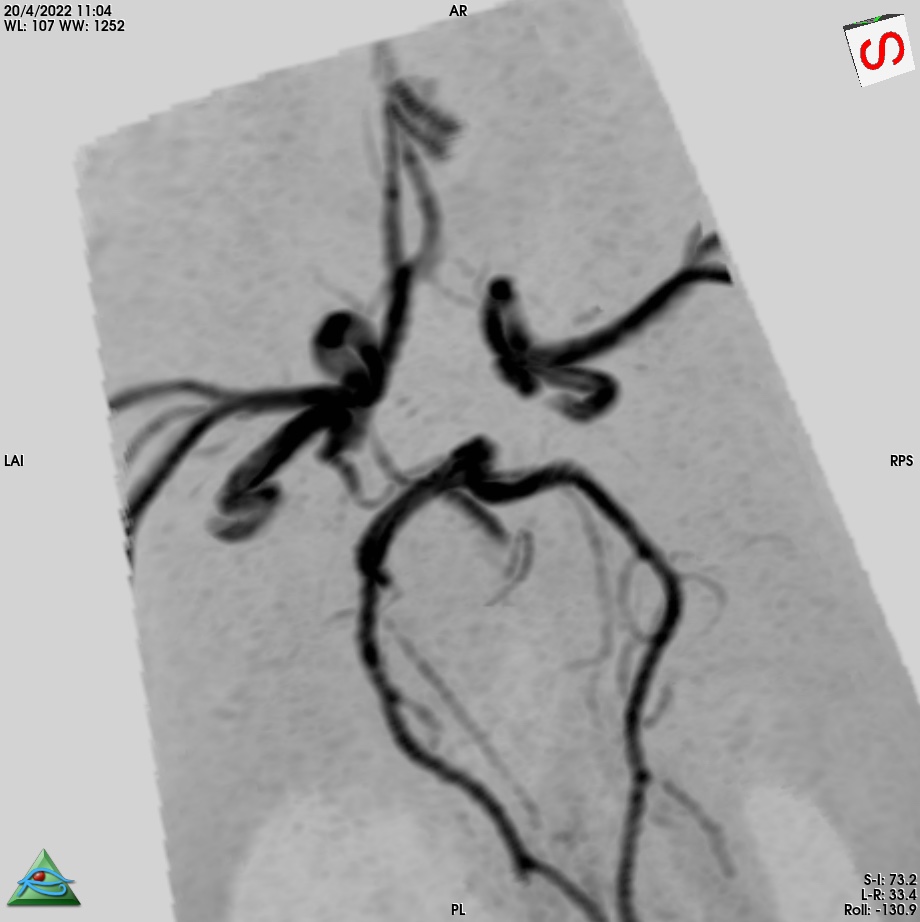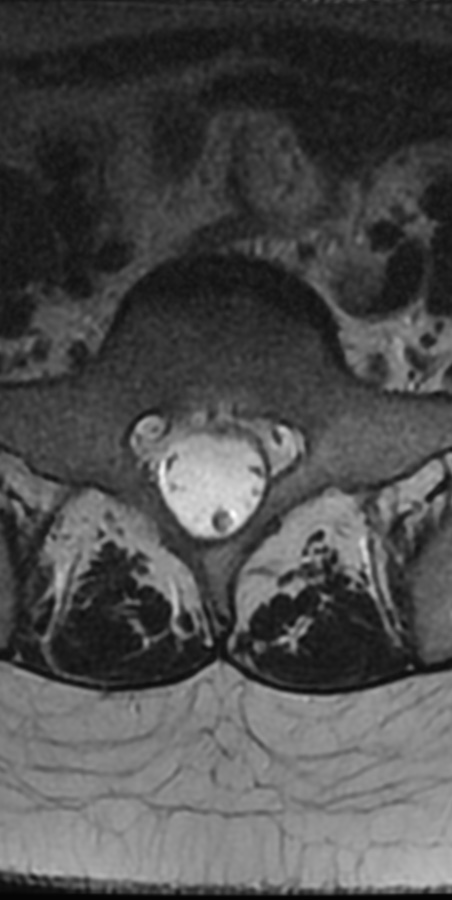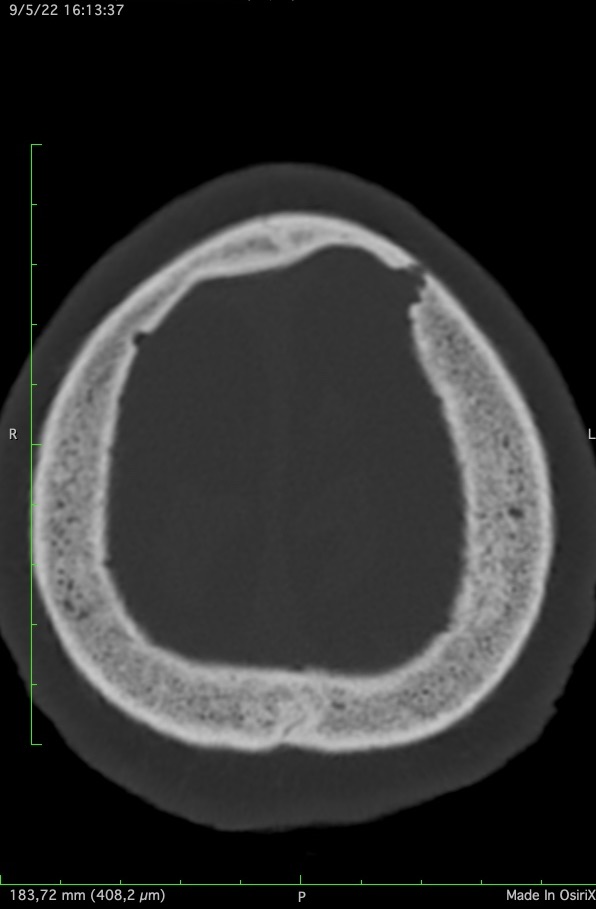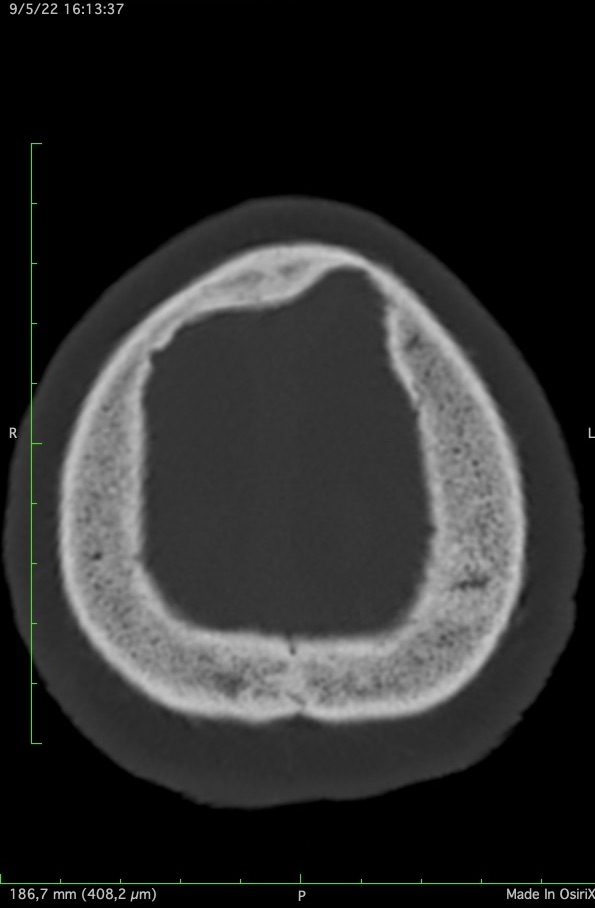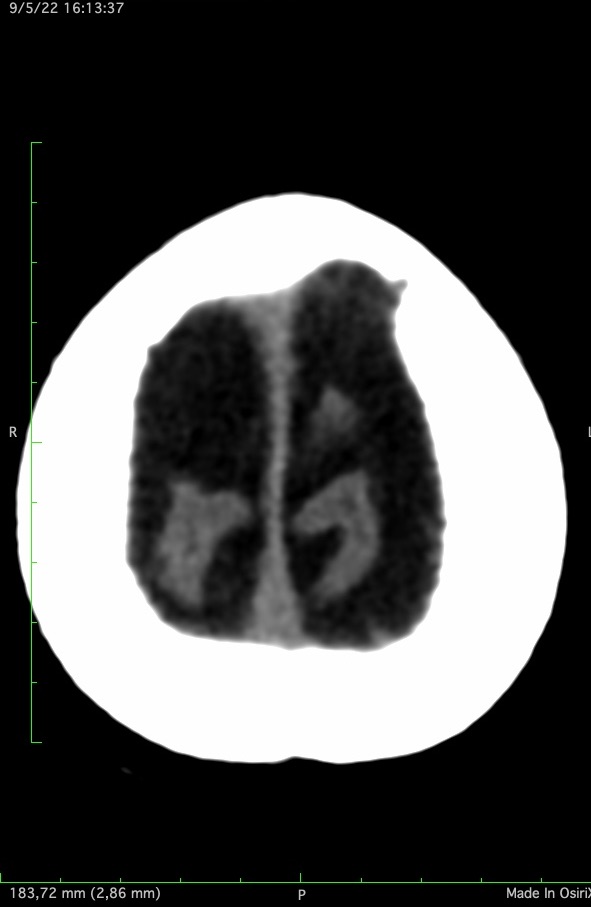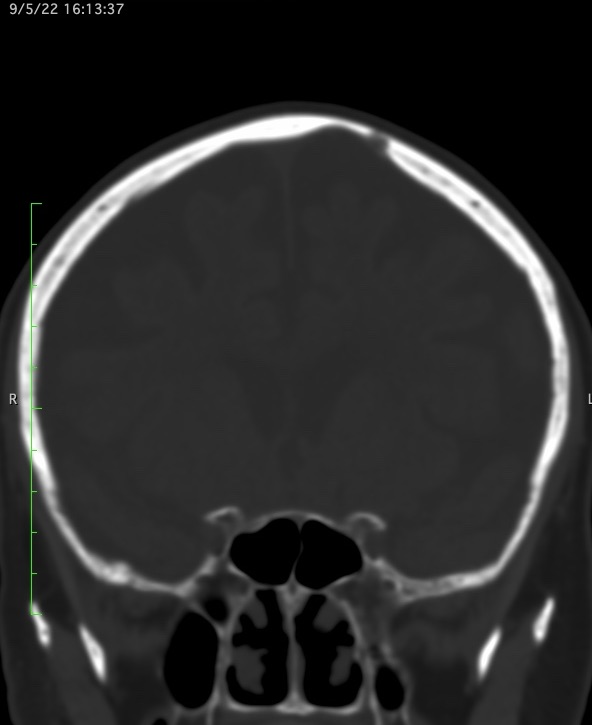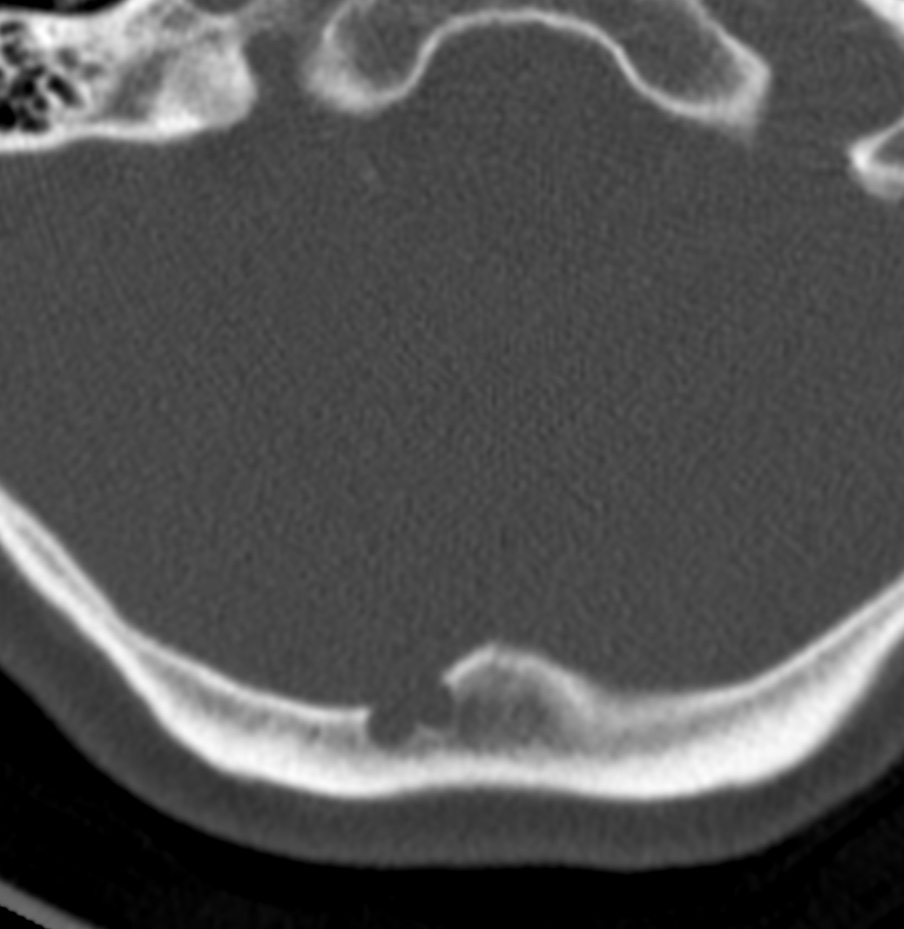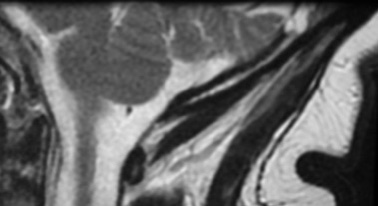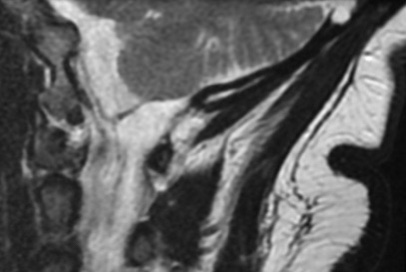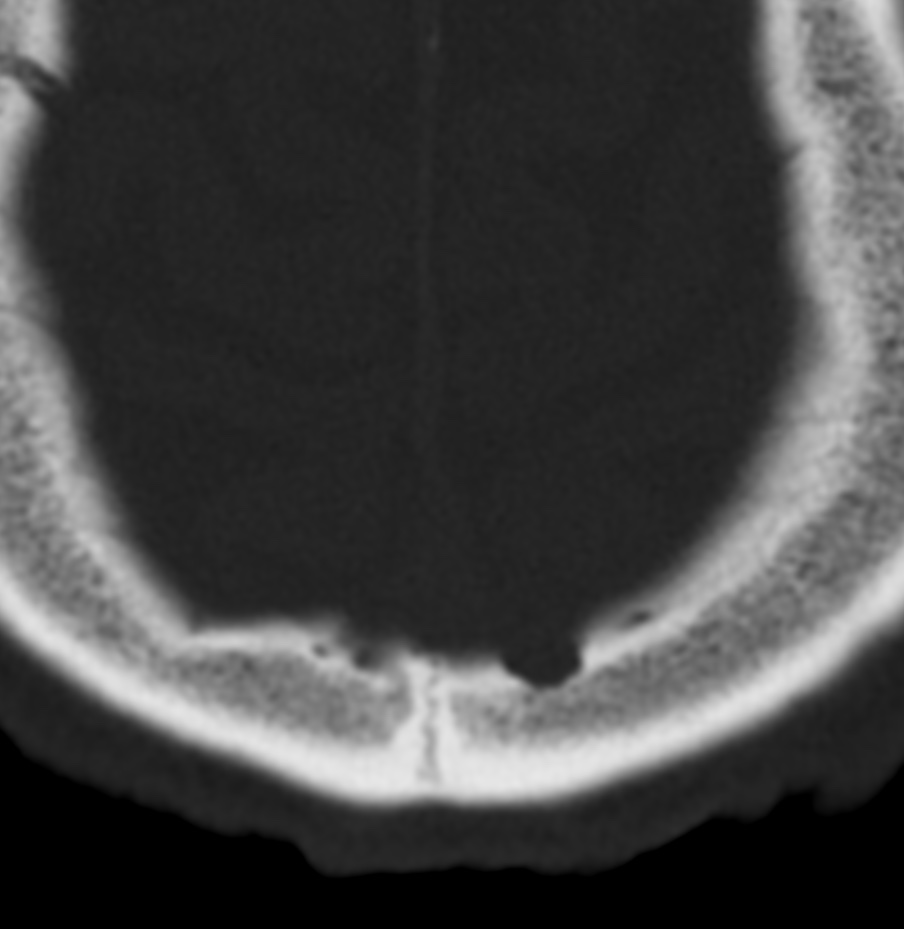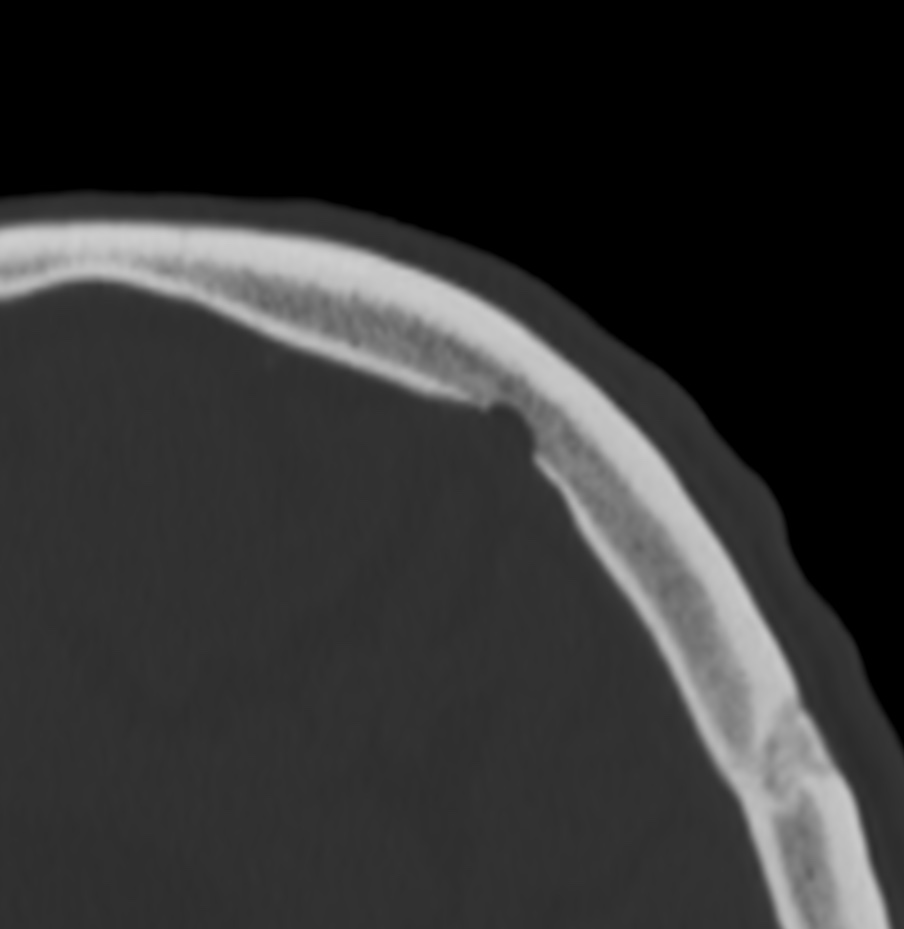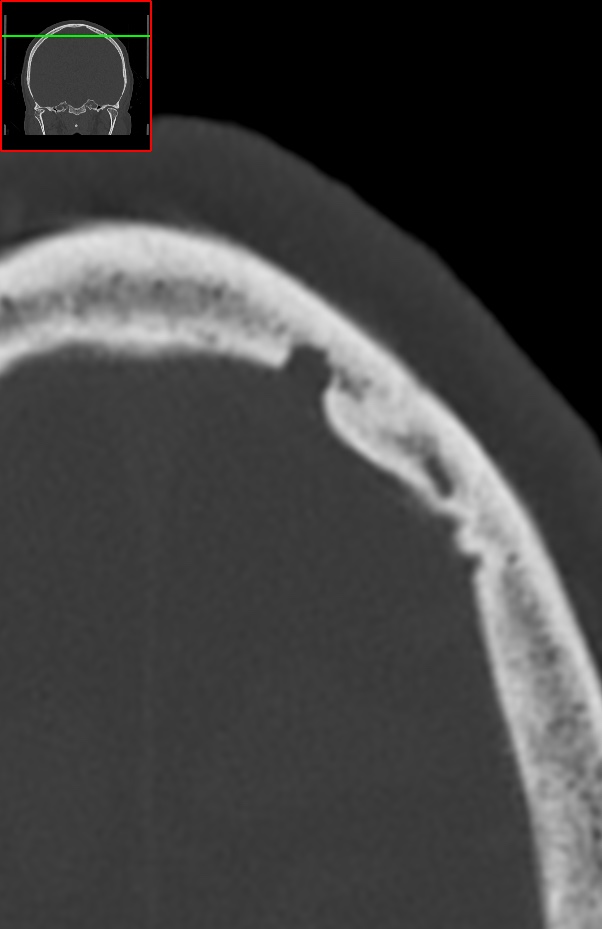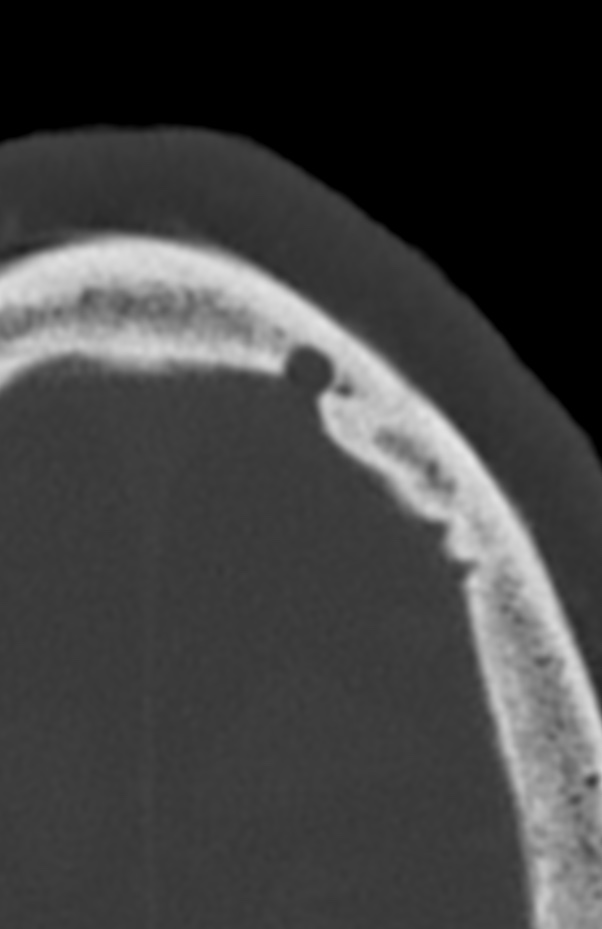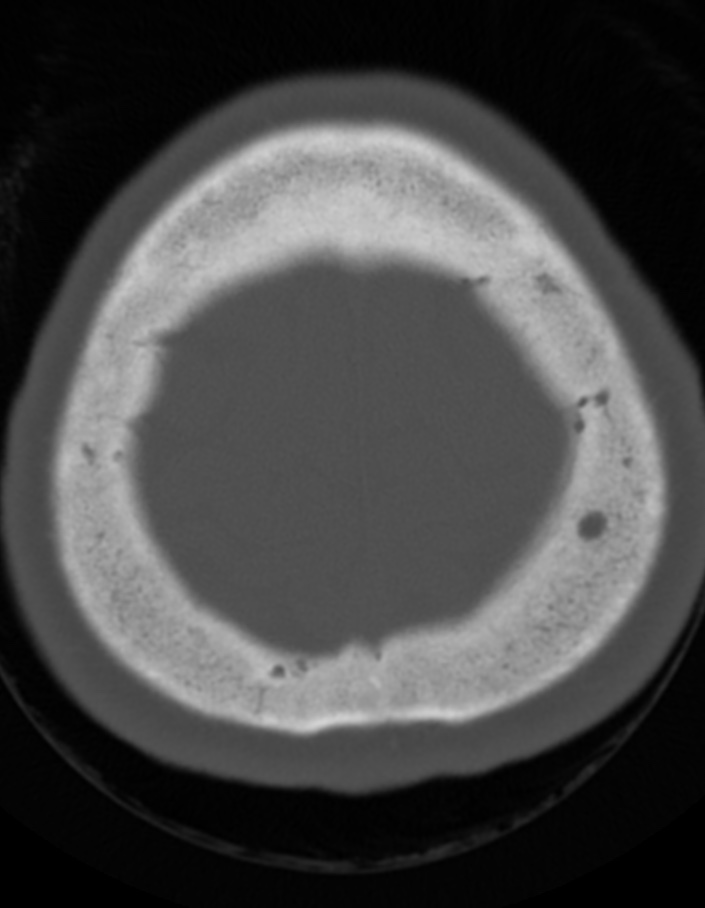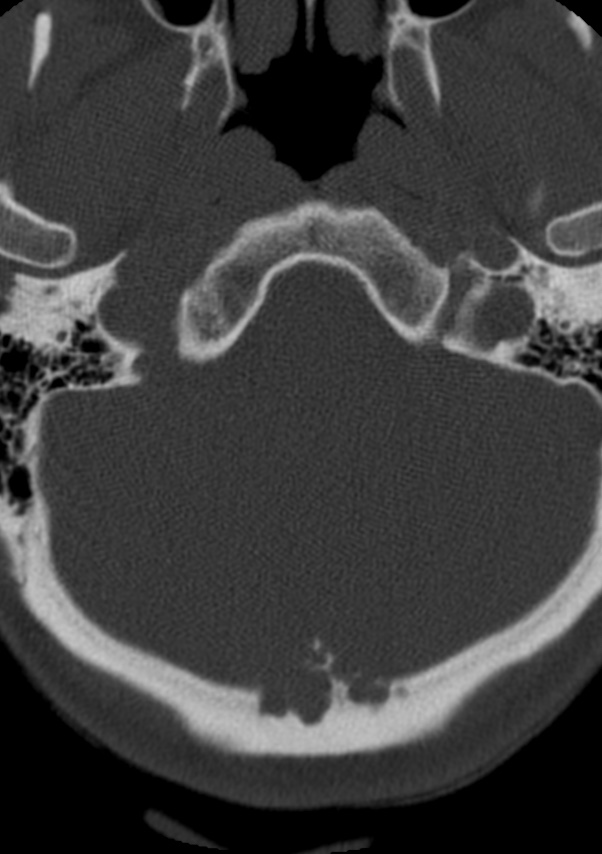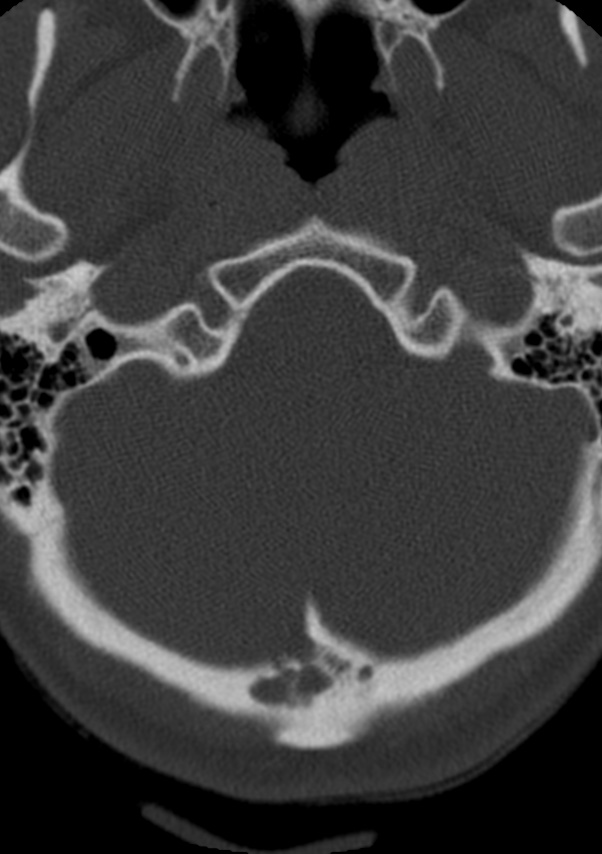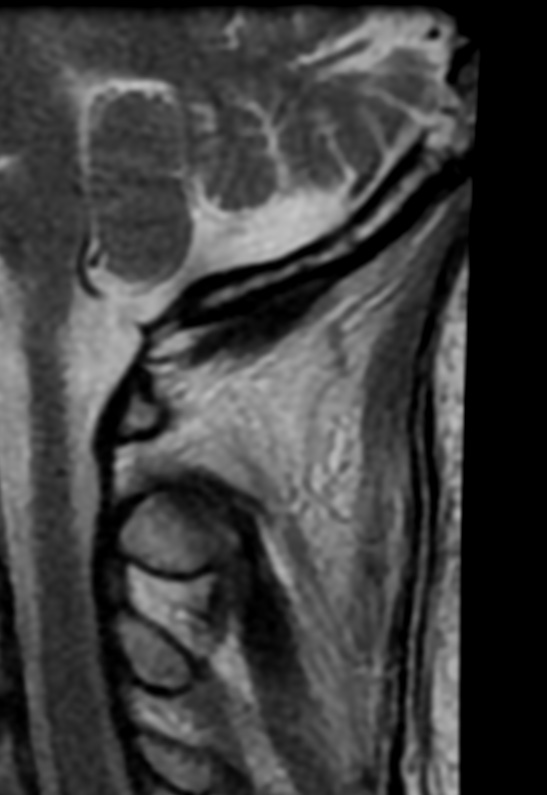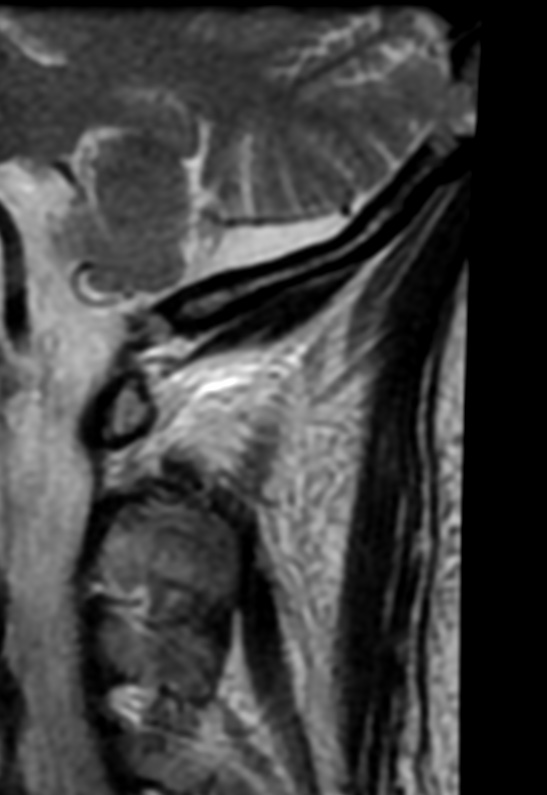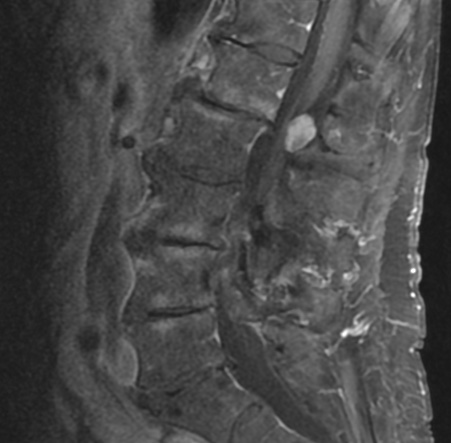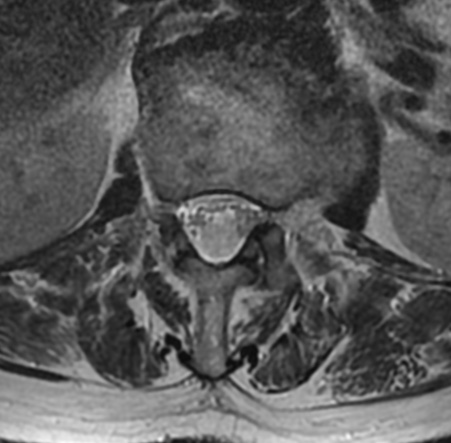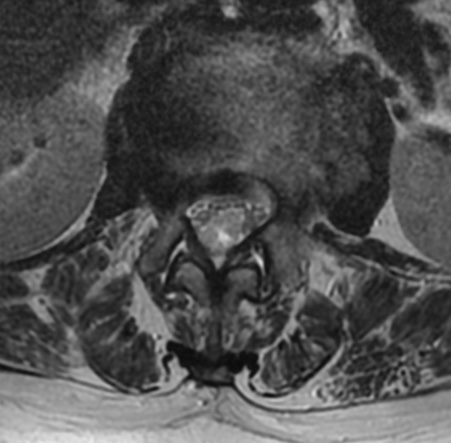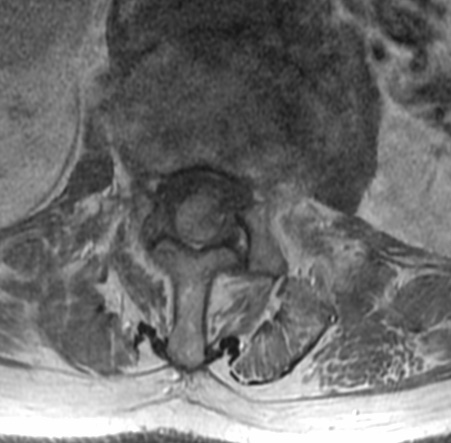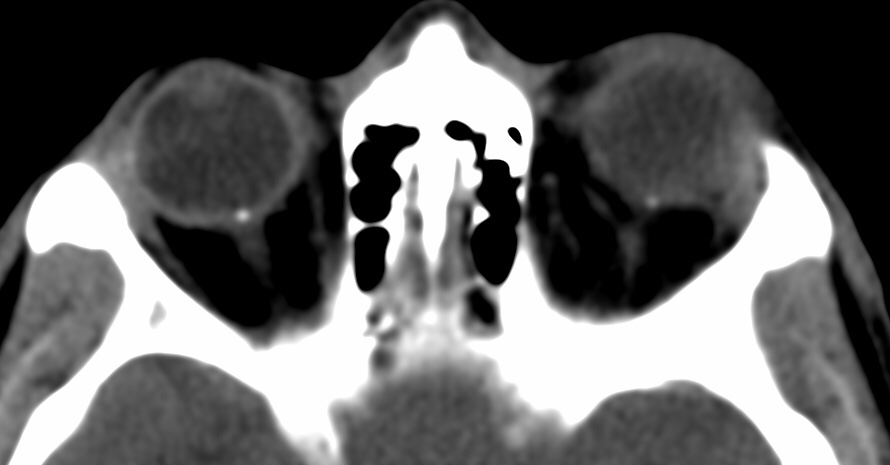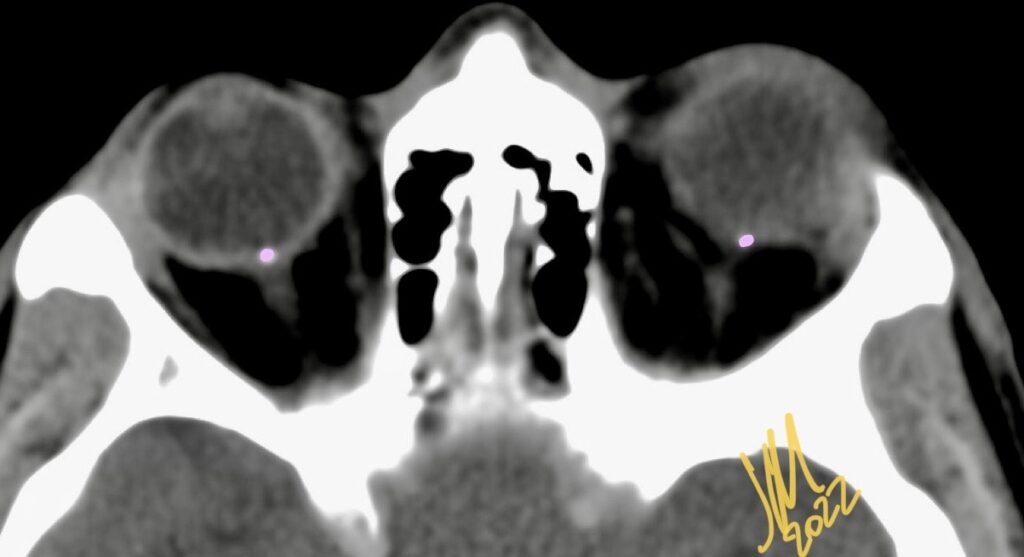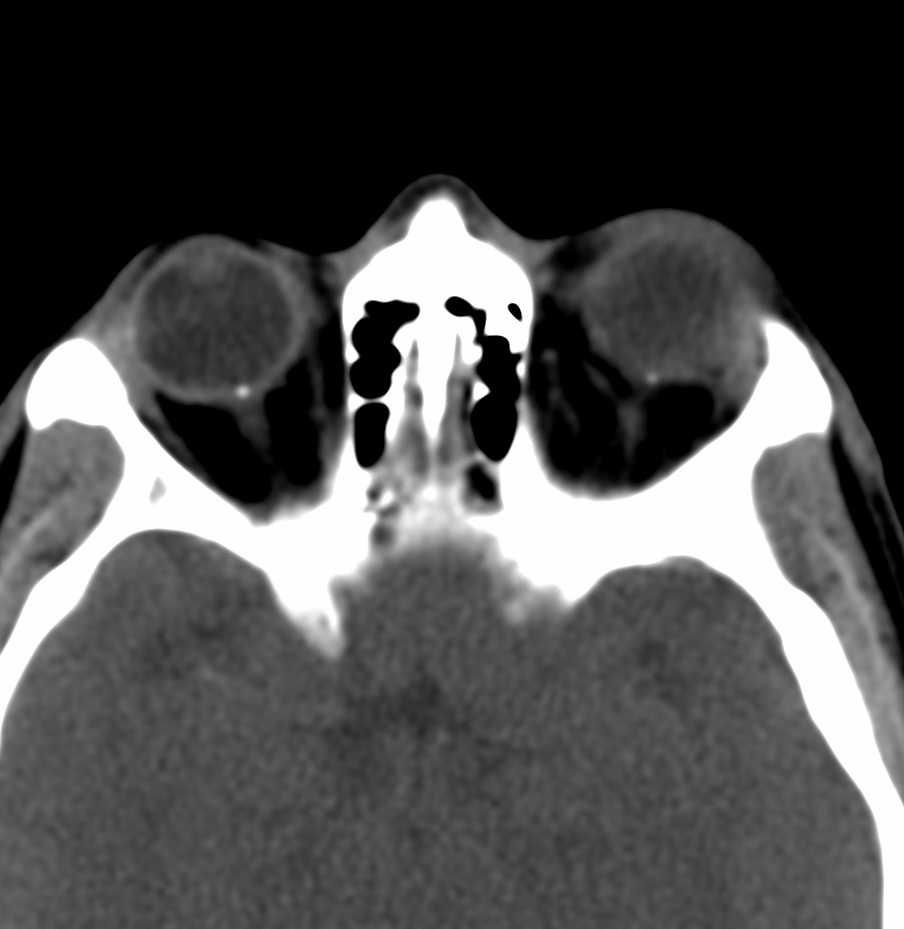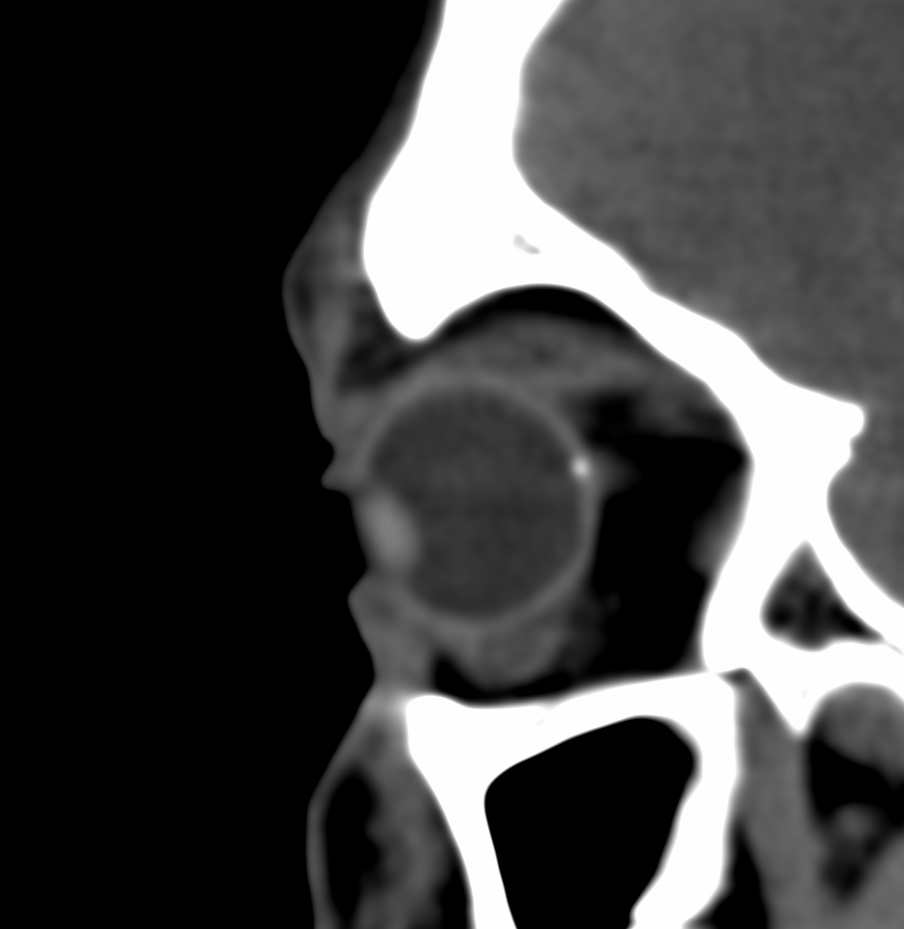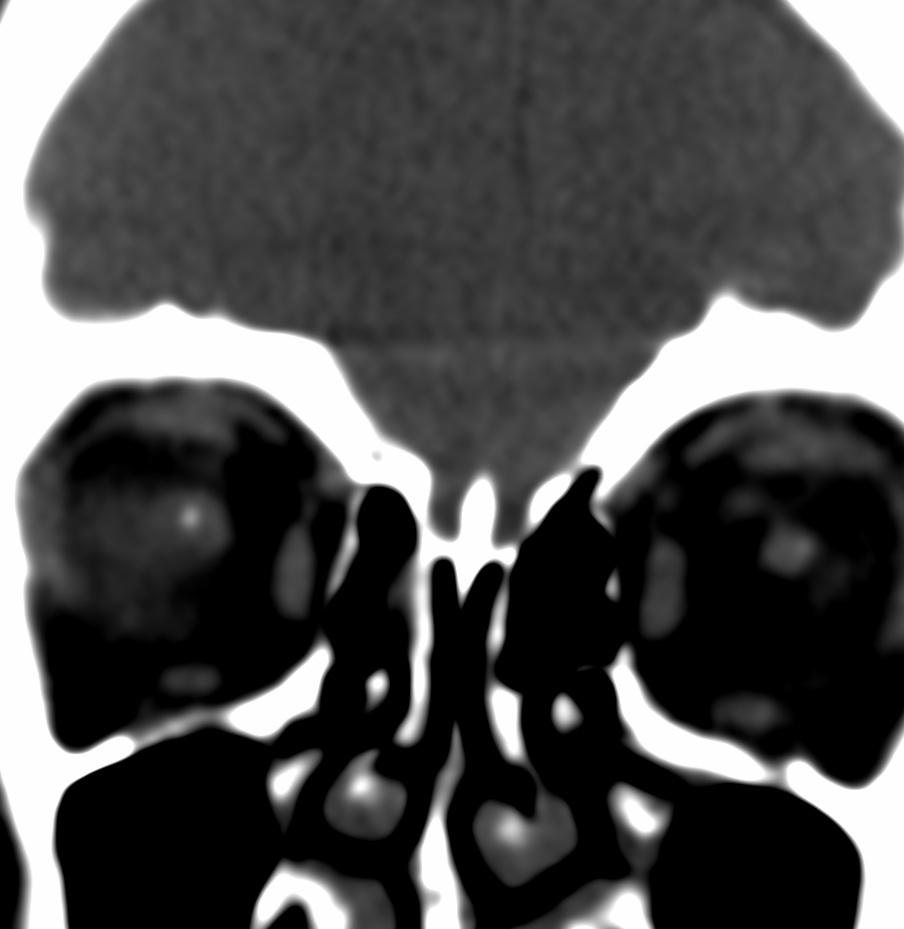
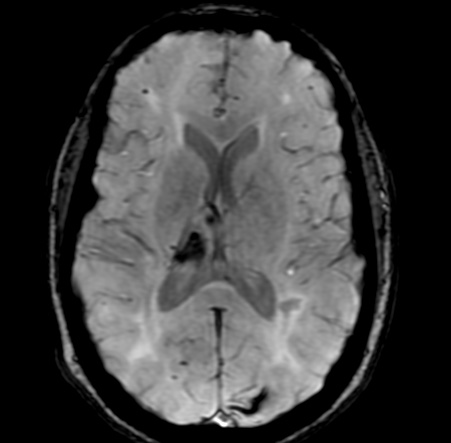
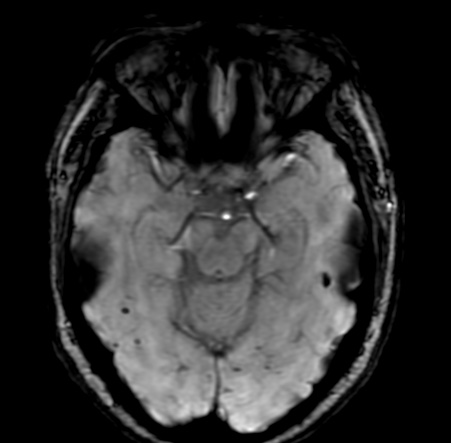
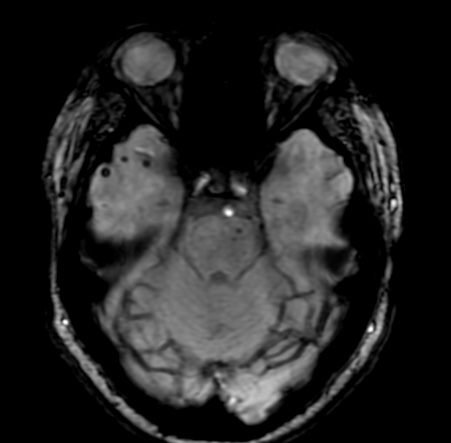
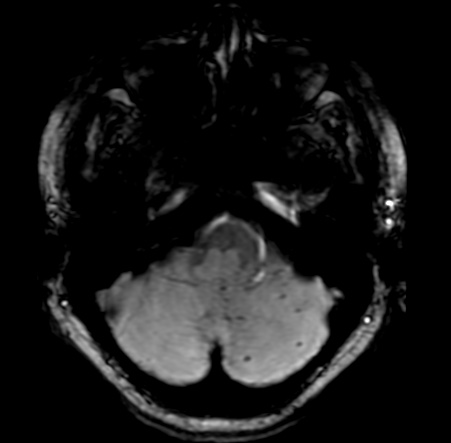
Cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is the most common genetic cause of stroke. In addition to ischemic stroke, CADASIL predisposes to development of cerebral microbleeds (CMB).
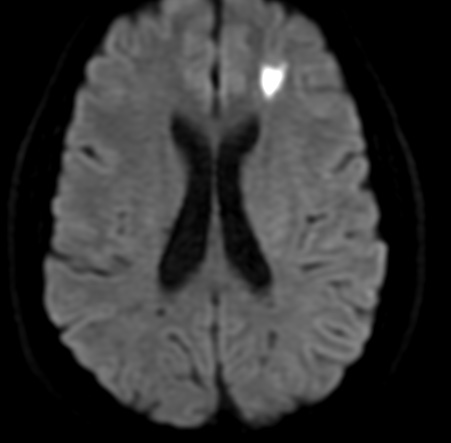
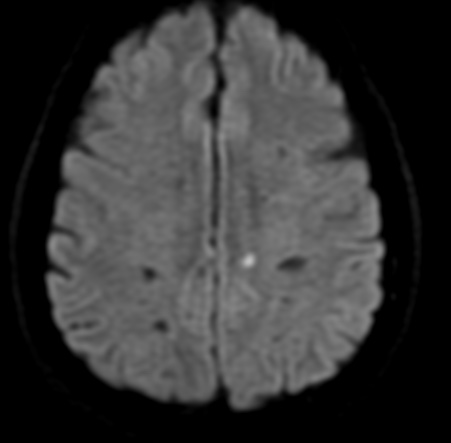
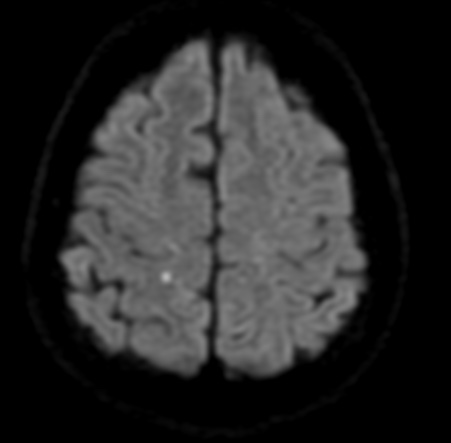
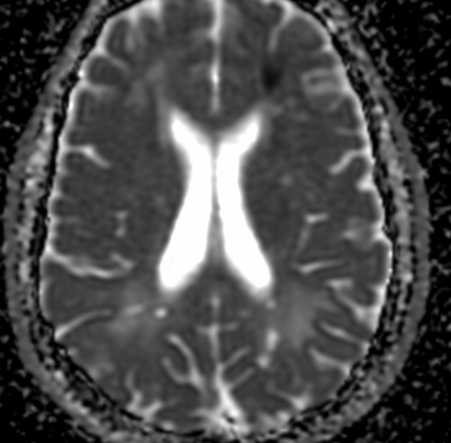
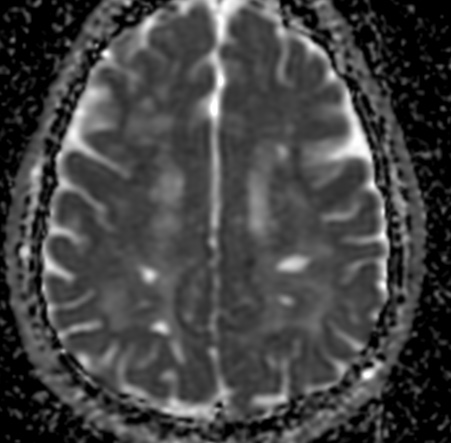
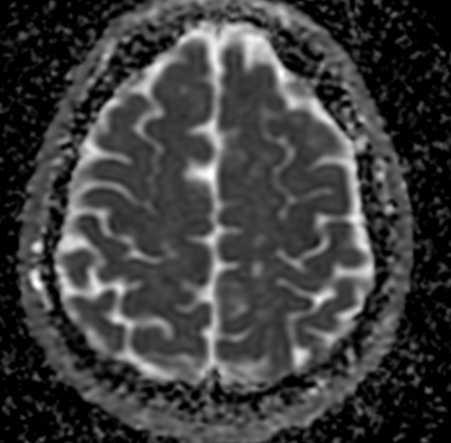
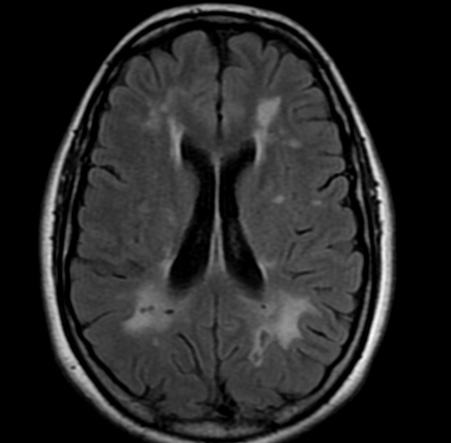
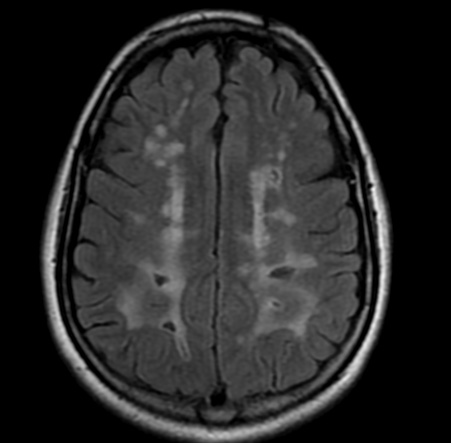
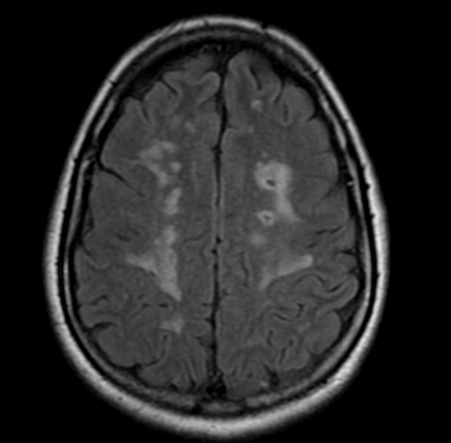
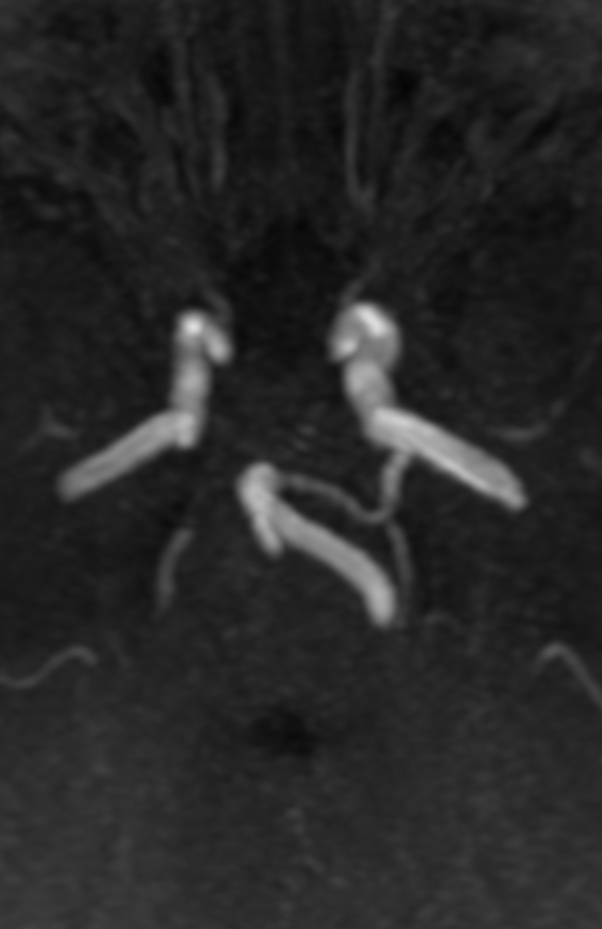
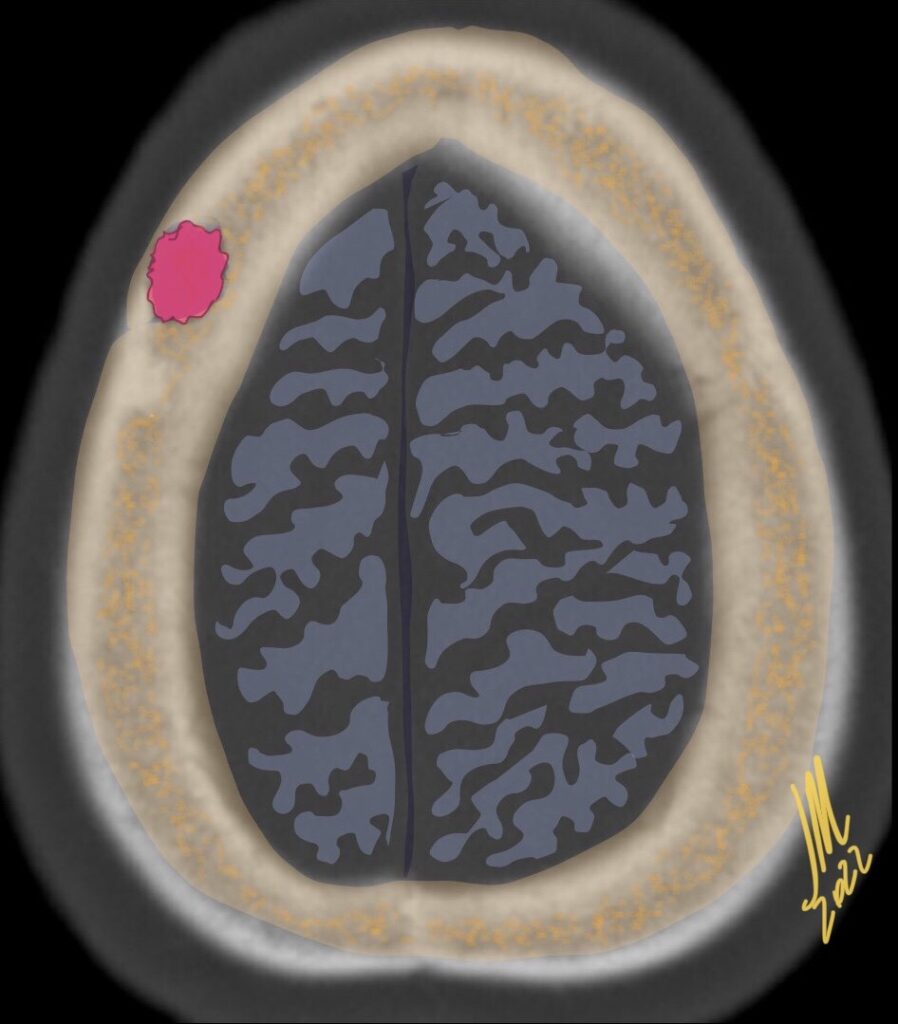
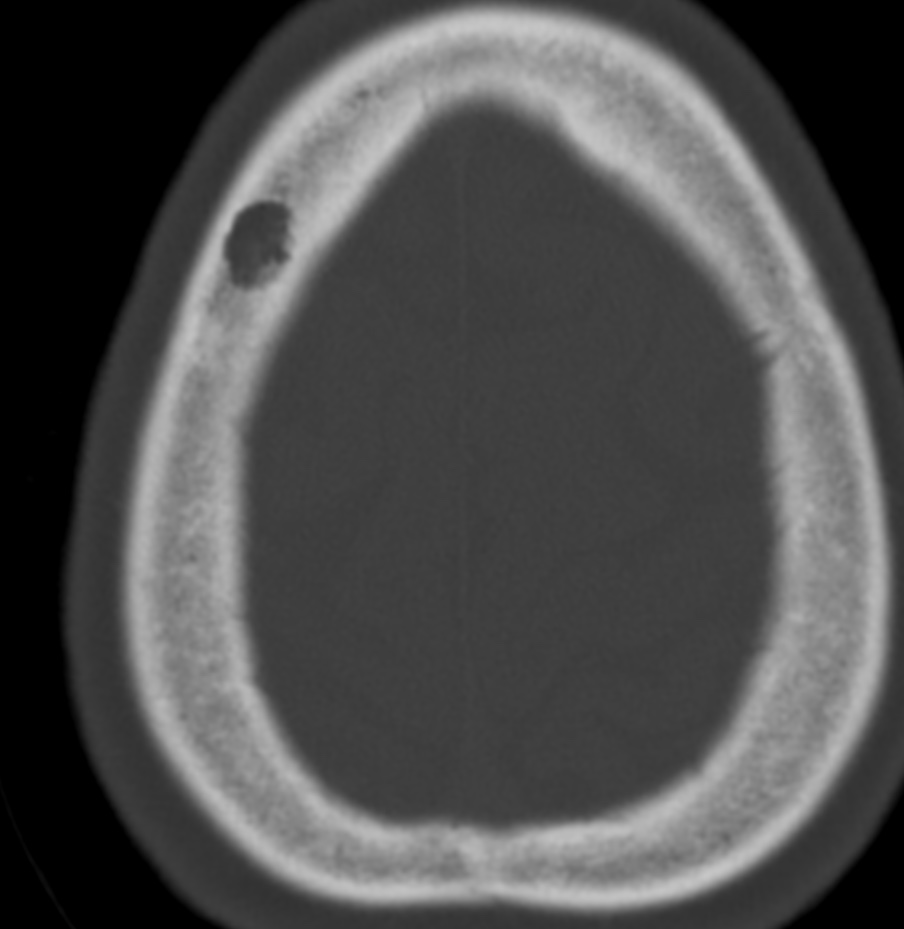
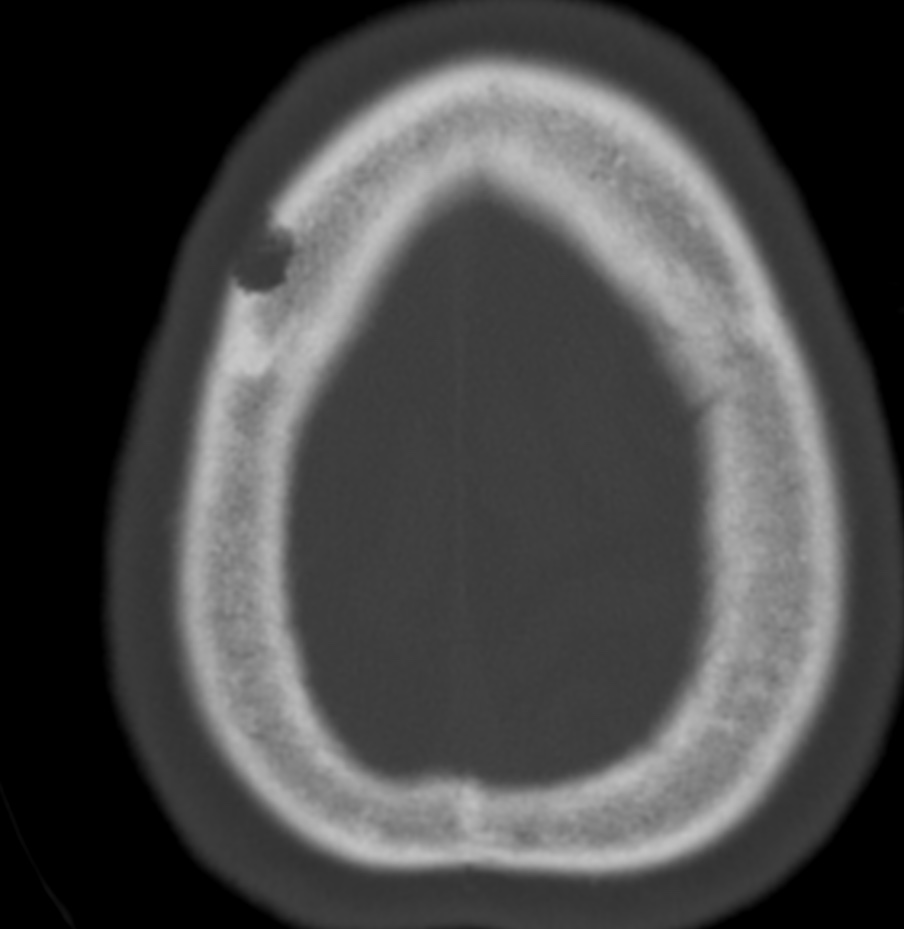
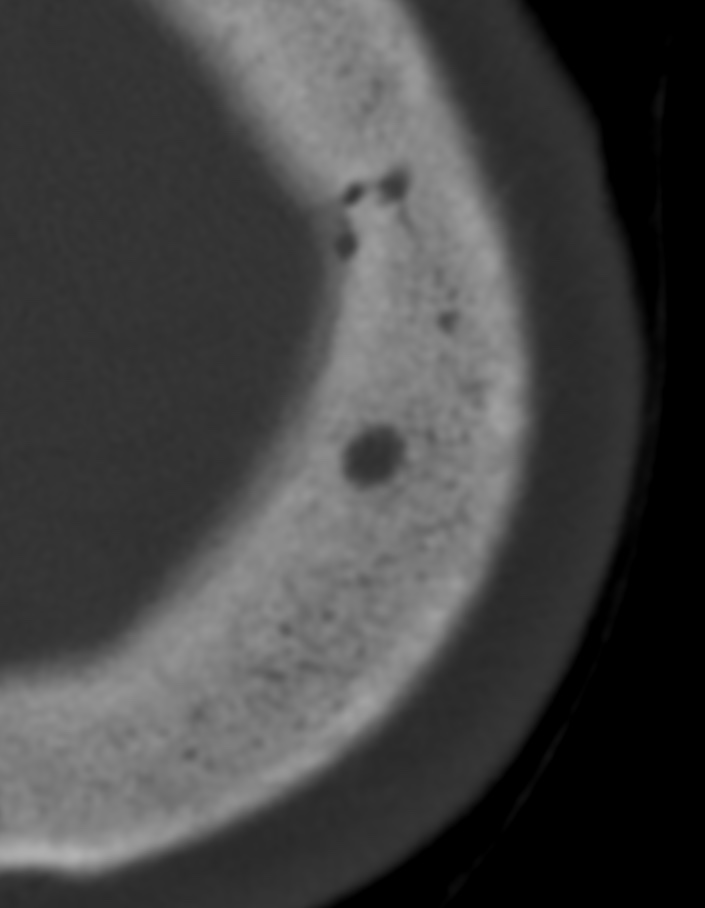
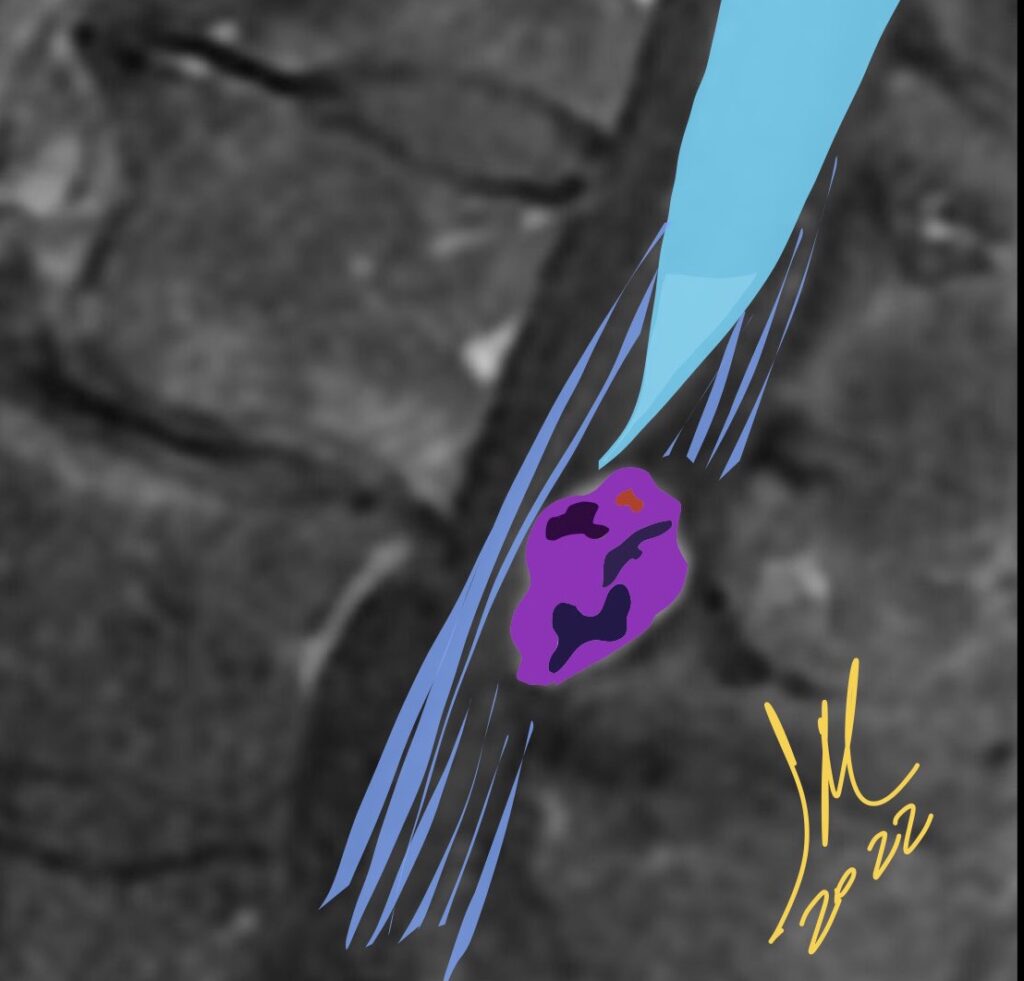
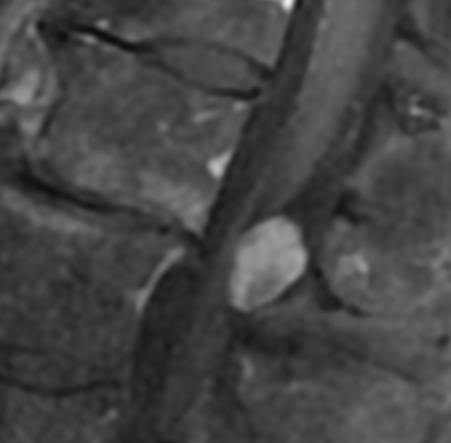
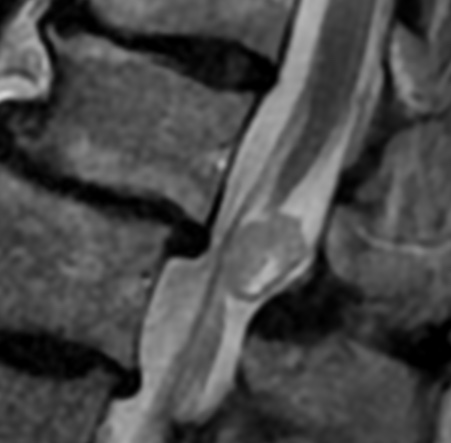
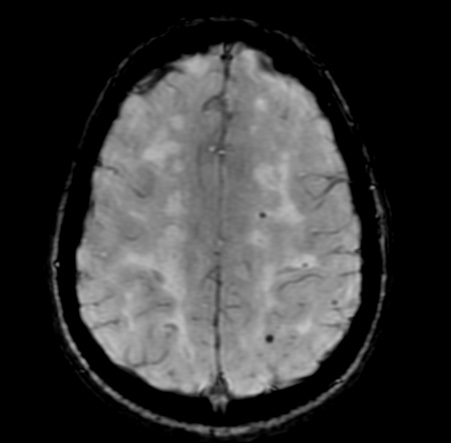
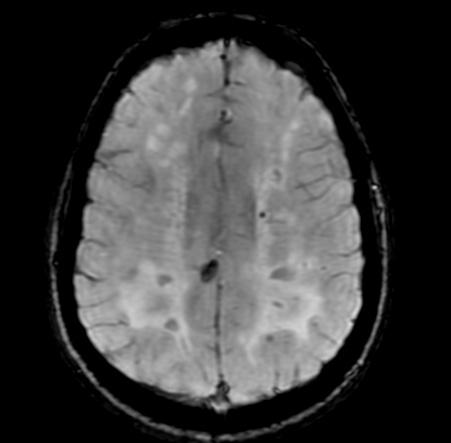
CMB are well-defined MRI-demonstrable brain lesions consisting of tiny perivascular hemosiderin deposits, detectable using T2*-weighted gradient echo or susceptibility-weighted imaging (SWI). CMB are associated with hypertension, cerebral amyloid angiopathy (CAA), and chronic kidney disease. CMB are also associated with intracerebral hemorrhage (ICH), which accounts for 20–30% of stroke in Asian countries such as Korea and Japan. Hypertension and CAA are the most common causes of ICH, and CAA is known to be associated with apolipoprotein E (ApoE)-ε4 genotype.
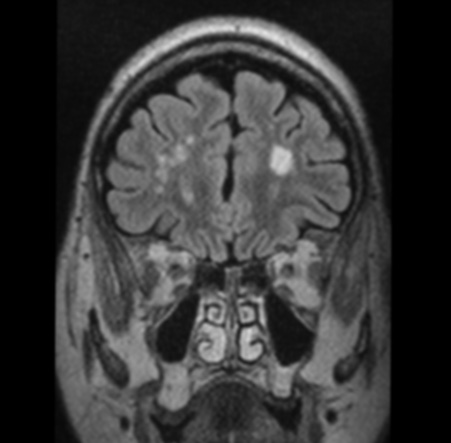
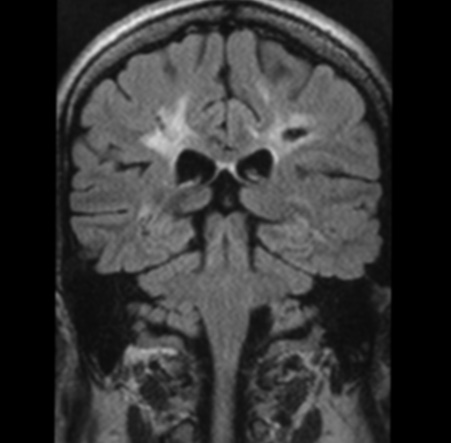
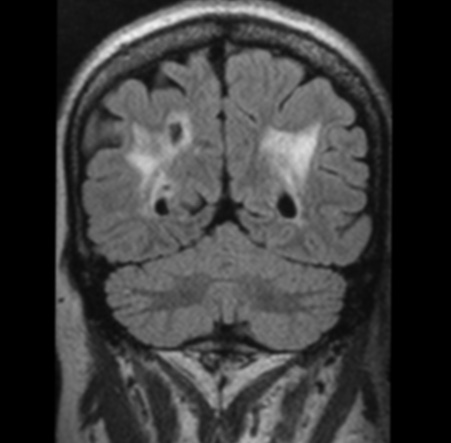
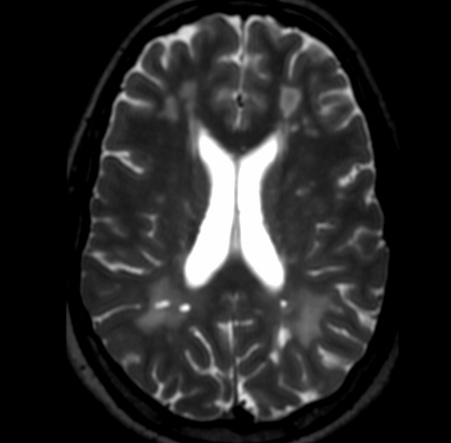
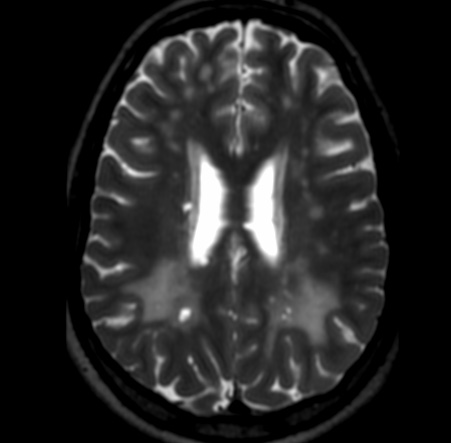
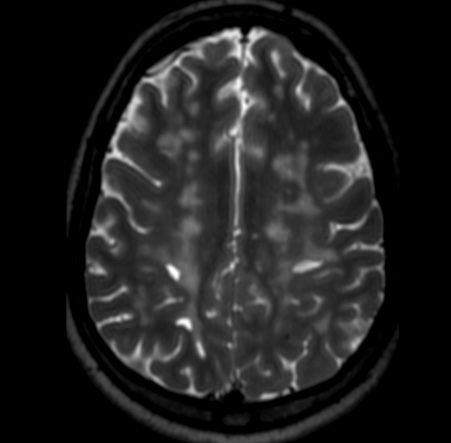
Intracerebral hemorrhage (ICH) has been described only sporadically for patients with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). However, cerebral microbleeds (CMBs) were found in 31% to 69% of the patients with CADASIL, and this predicted an increased risk of ICH. In this study, the authors found that 25% of the symptomatic patients with CADASIL had ICHs, and their development was closely related to the number of CMBs.
Reference:
Front. Neurol., 15 May 2017 | https://doi.org/10.3389/fneur.2017.00203