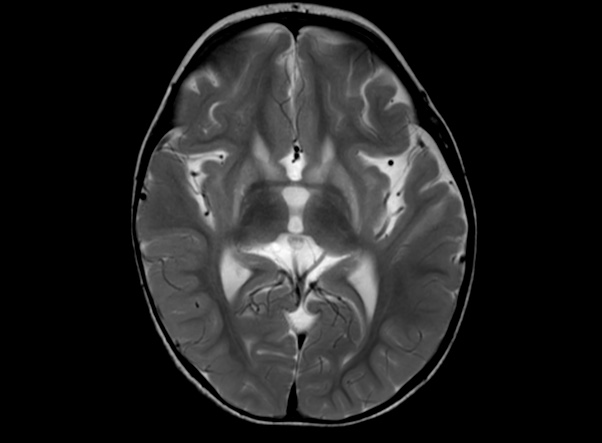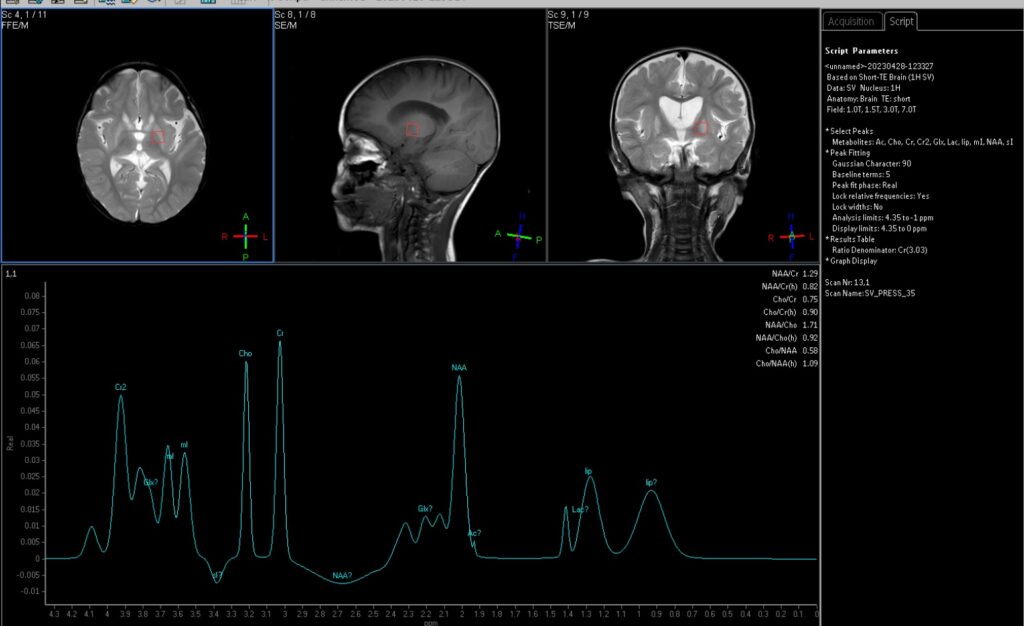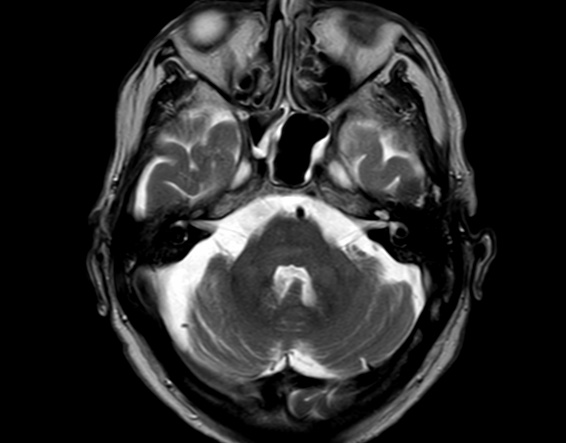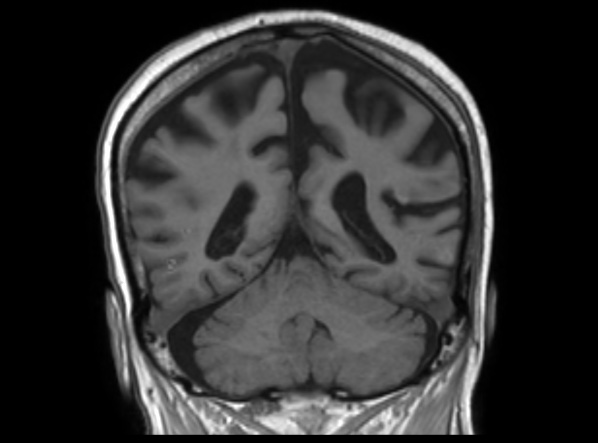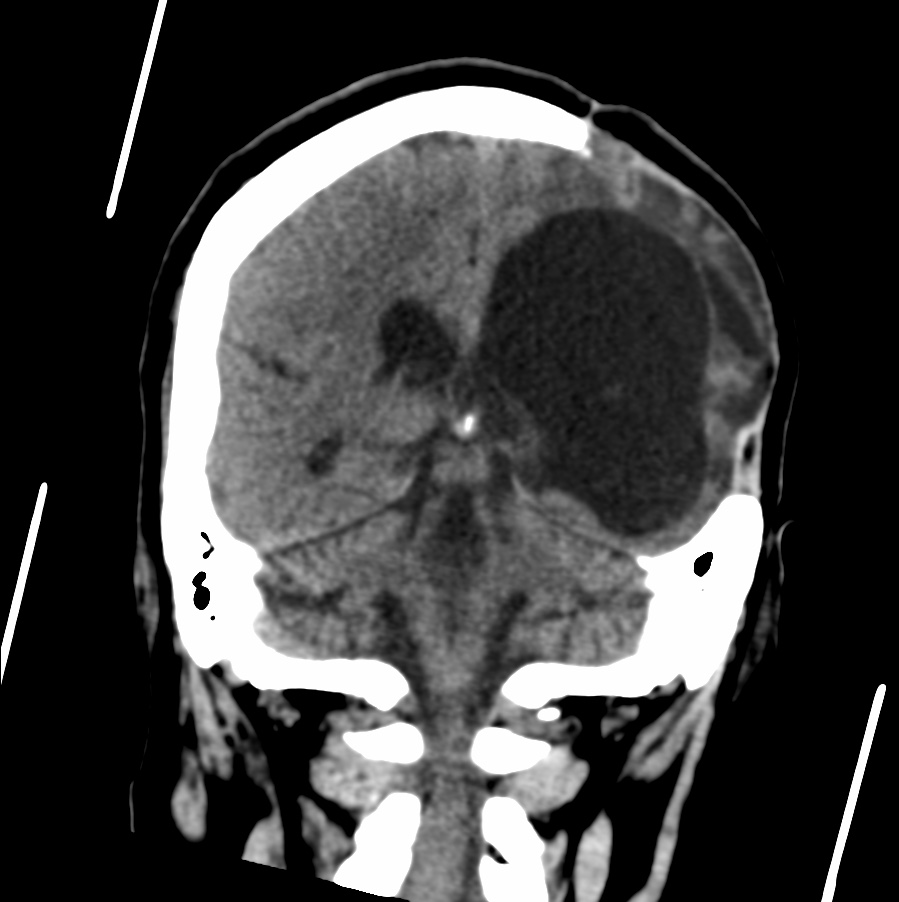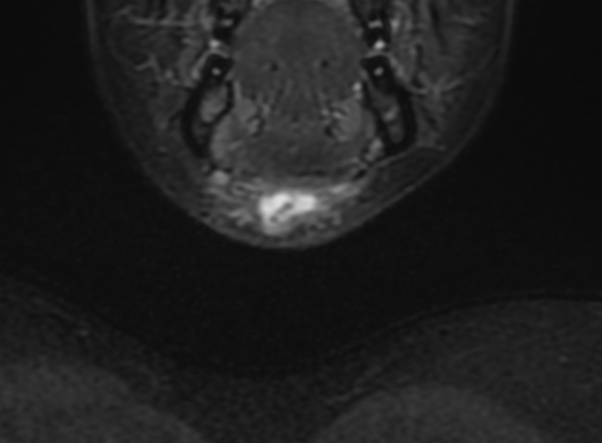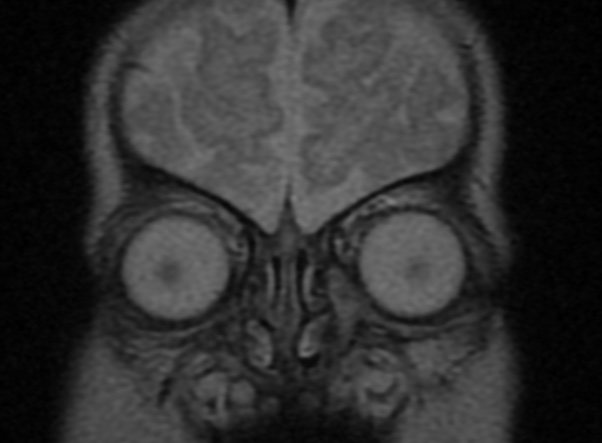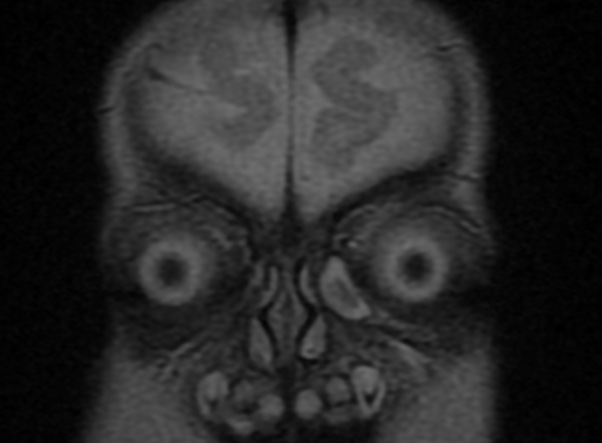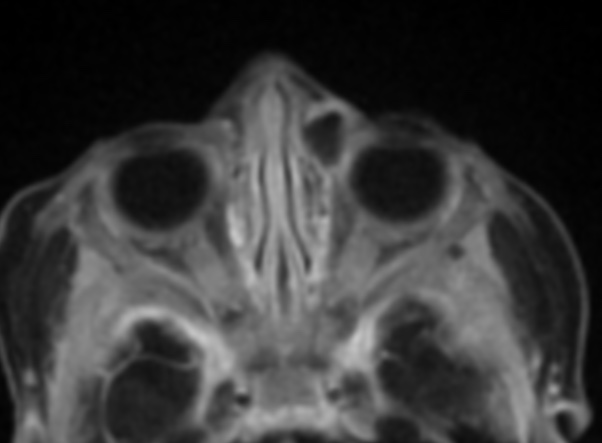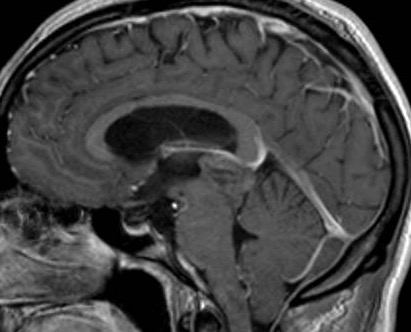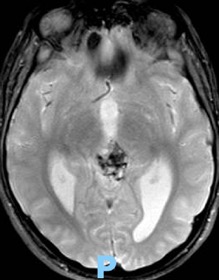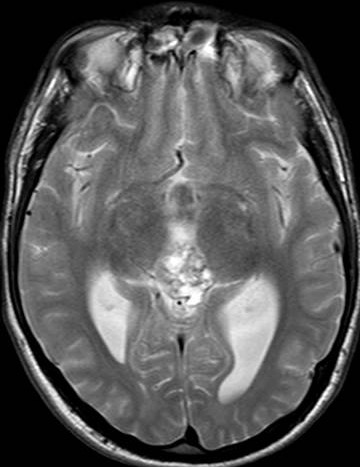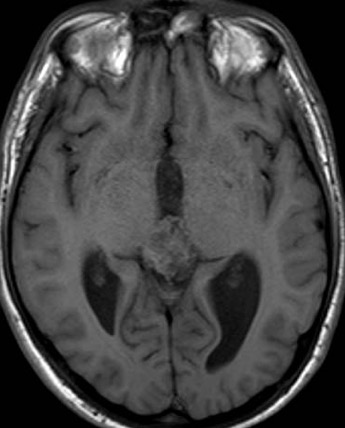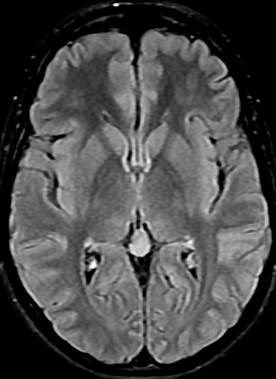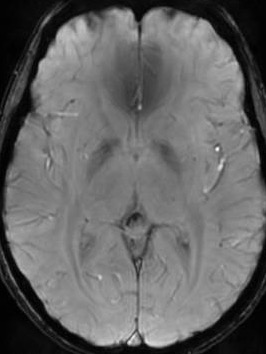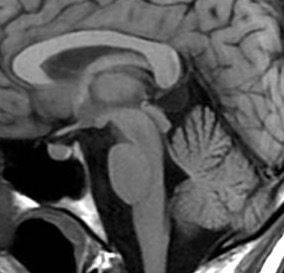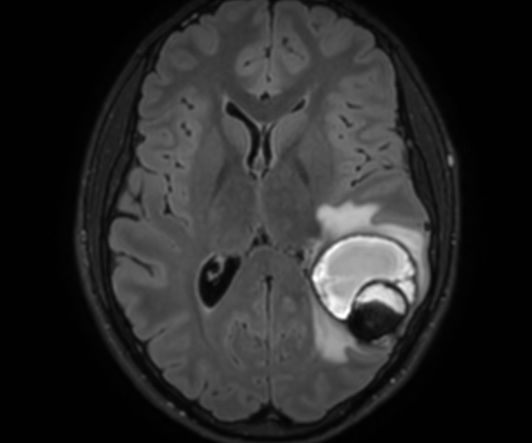
The cavernous malformation (CM), also known as cavernous angioma or cavernoma, is a vascular malformation characterized by the presence of sinusoid-like capillary vessel containing blood in very sluggish circulation.
CMs vary in size from a few millimeters to a few centimeters. Few data can be found about the size of these malformations. Kim et al. reported the size of cavernoma between 1mm and 75 mm, with a mean size 14.2 mm. The majority of cavernous malformations are small but it may reach significant size. Unlike giant aneurysms, defined as having a diameter of at least 25 mm, no threshold dimension has been accepted for giant cavernous malformation (GCM).
Lawton et al., although arbitrary, defined a GCM as a cavernoma with a diameter greater than 6 cm. GCMs are very rare and usually not considered in the differential diagnosis of large tumor.
Cerebral CMs rarely attain large dimension. The mechanism by which they enlarge is probably recurrent bleeding, followed by organization of the clot, pseudocapsule formation, and secondary expansion. However, it was also reported that CMs can show expansile growth without any evidence of a hemorrhagic event and mimic neoplasm.
Reference: