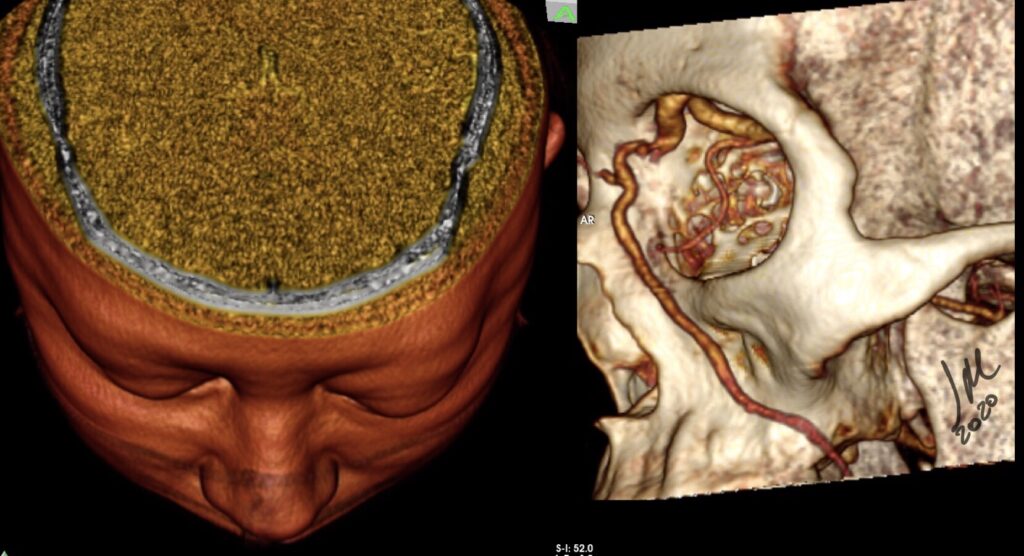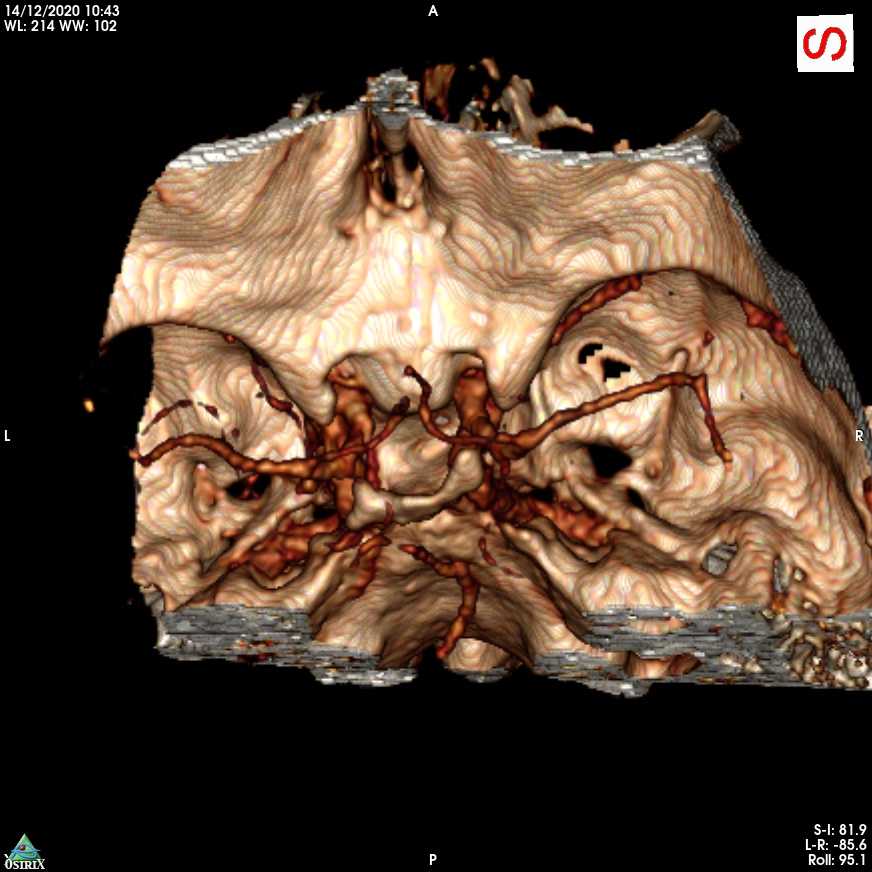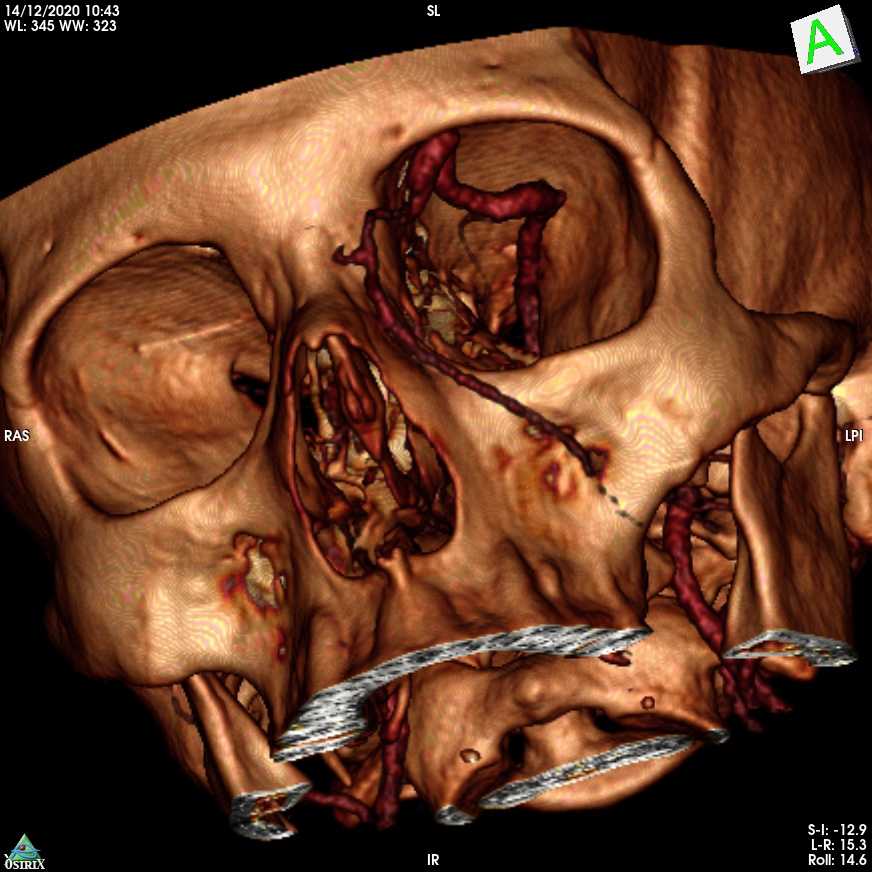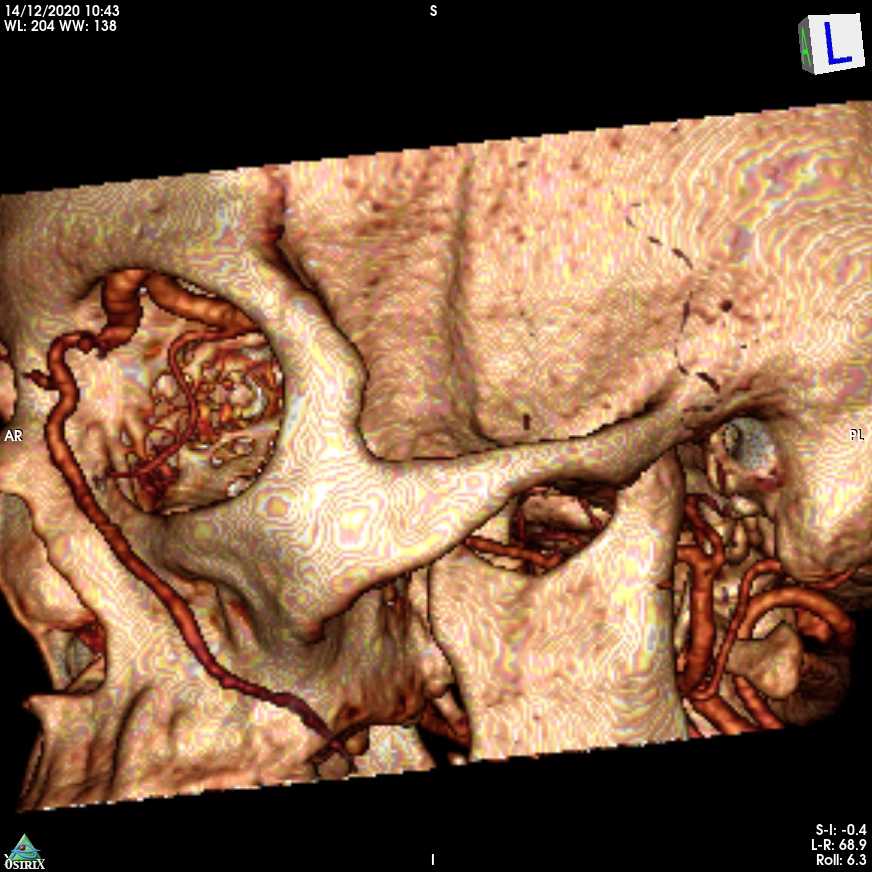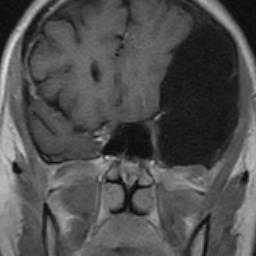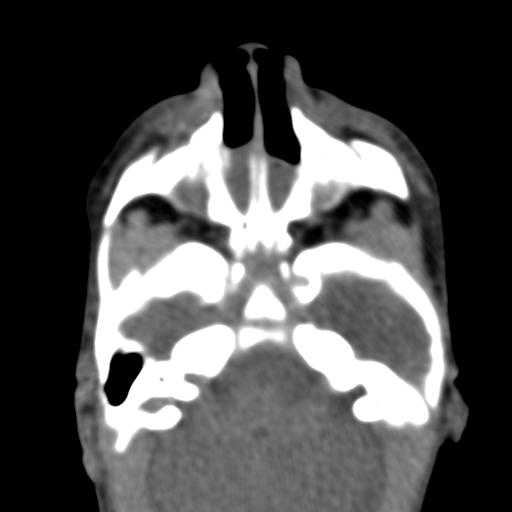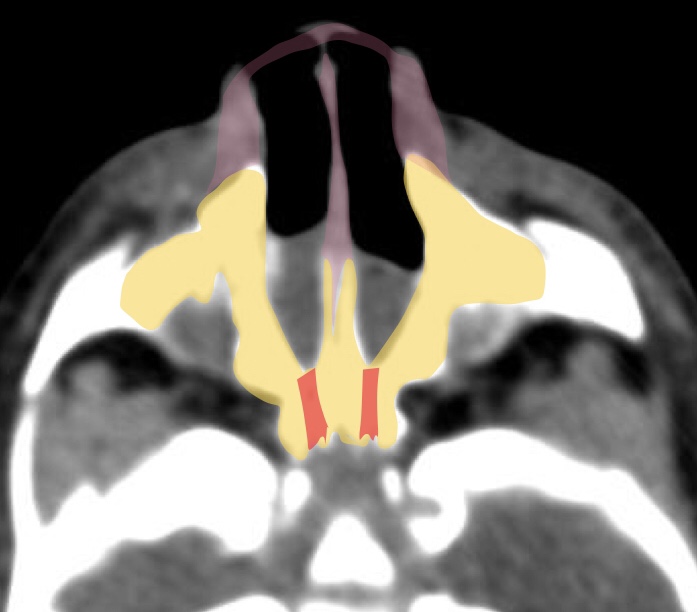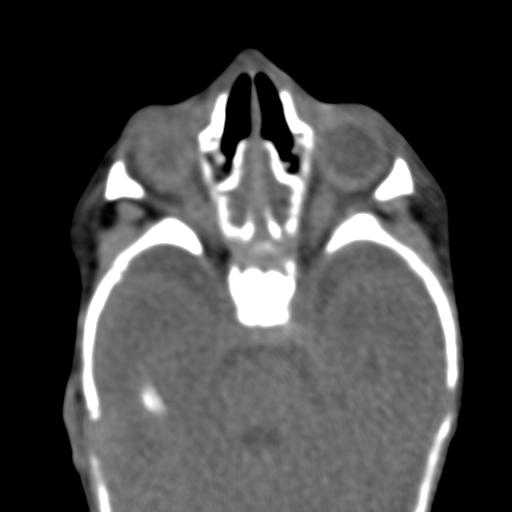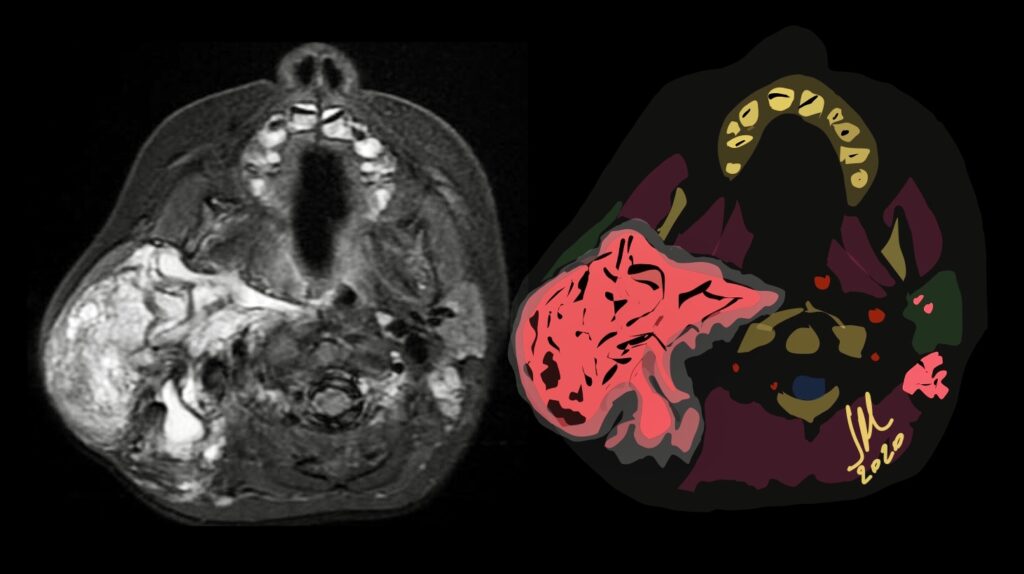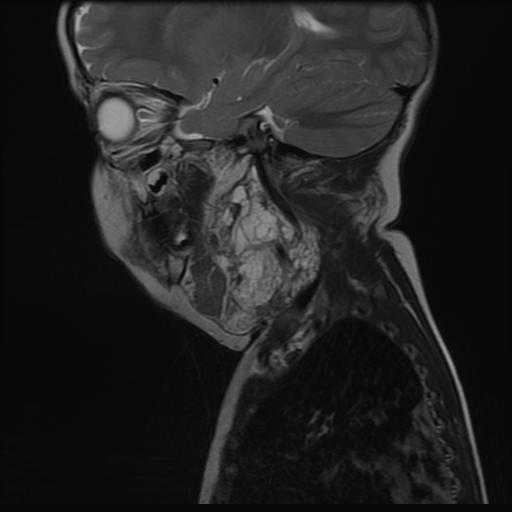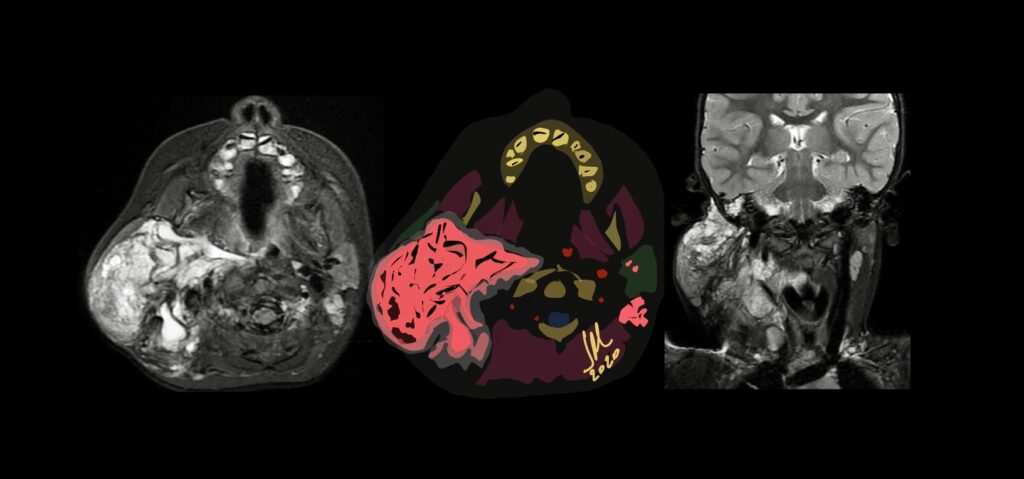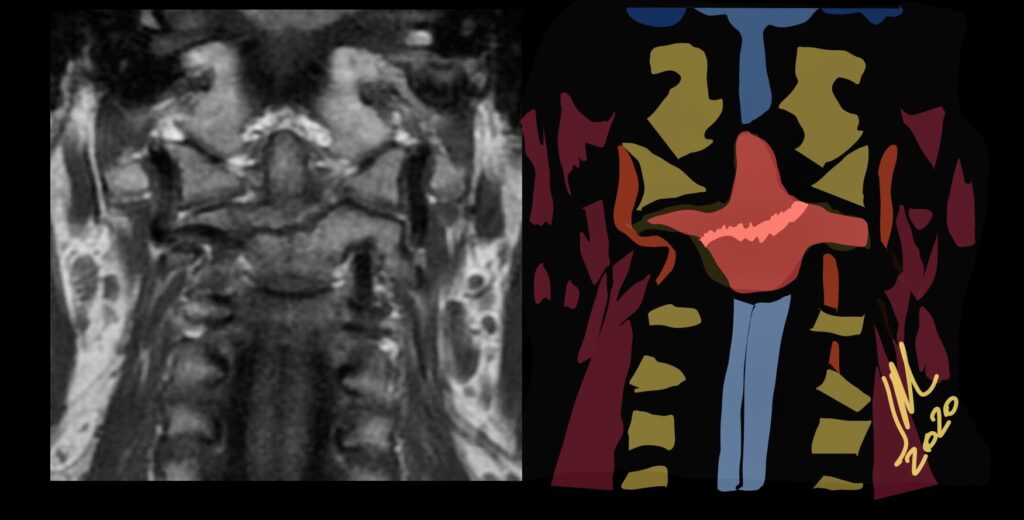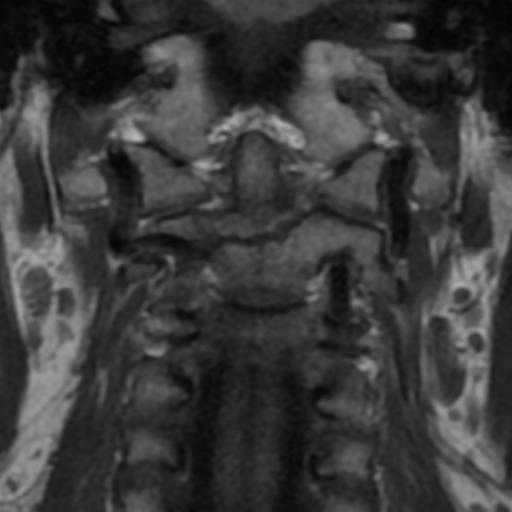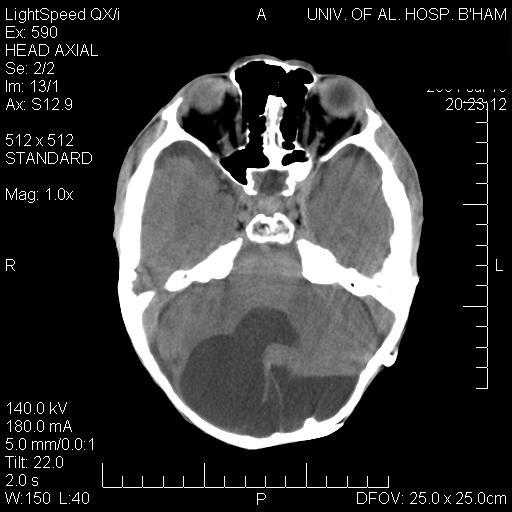
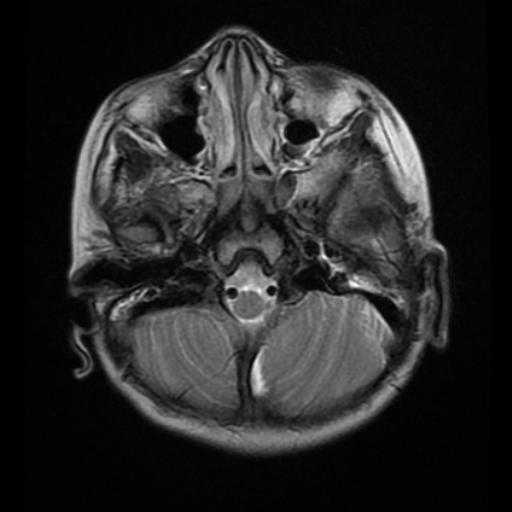
Characteristic maxillofacial findings of acromegaly include thickening of the calvaria, more pronounced in the inner table, enlarged paranasal sinuses, most often the frontal sinus, resulting in frontal bossing, and enlargement of the mandible, which may lead to prognathism and gaps between the teeth. Diffuse and symmetric enlargement of the extraocular muscles has been described as part of the generalized organomegaly associated with acromegaly.
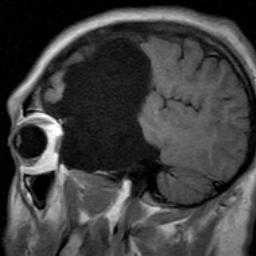
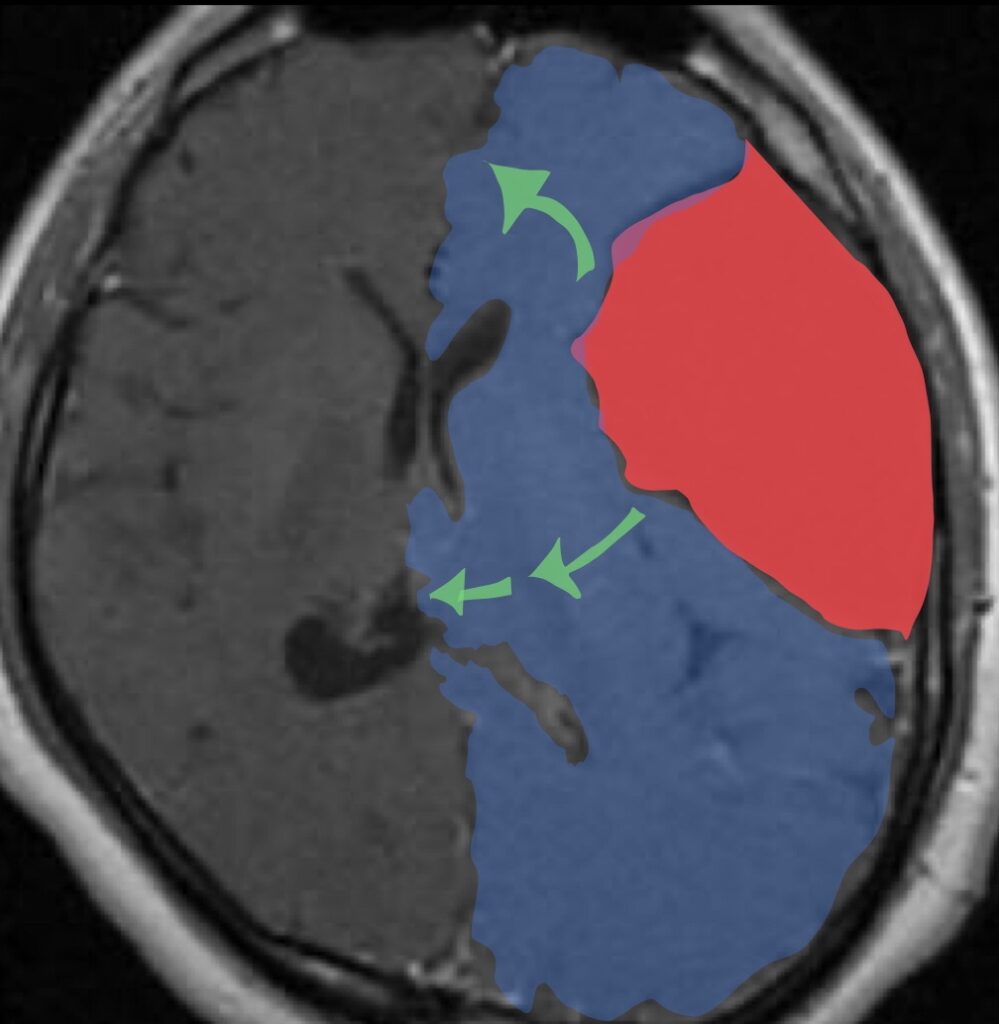
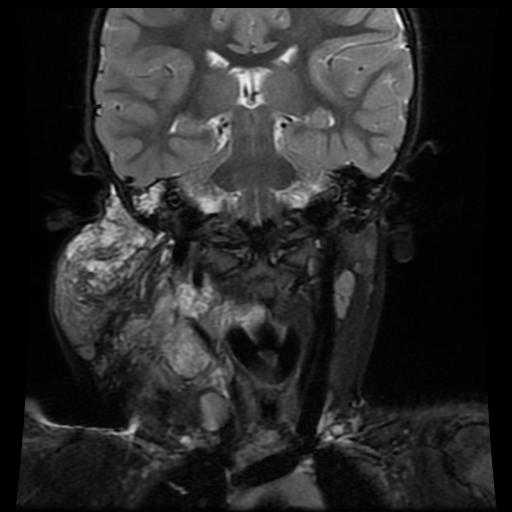
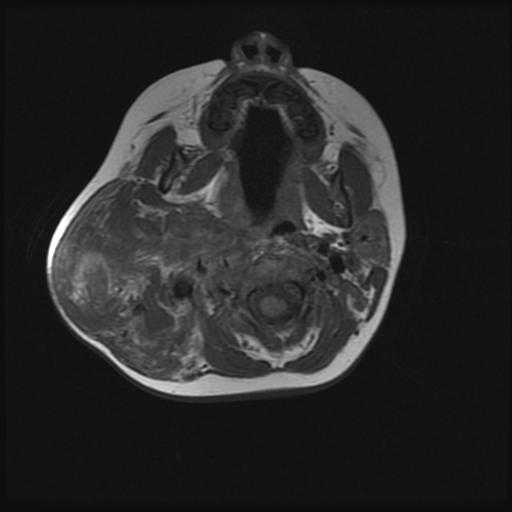
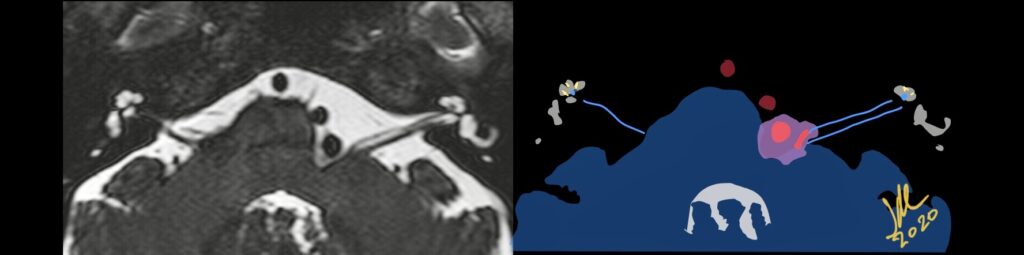
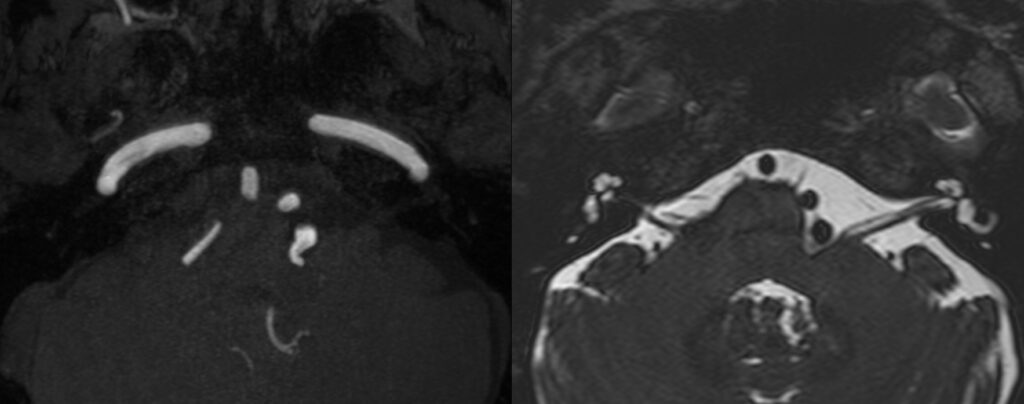
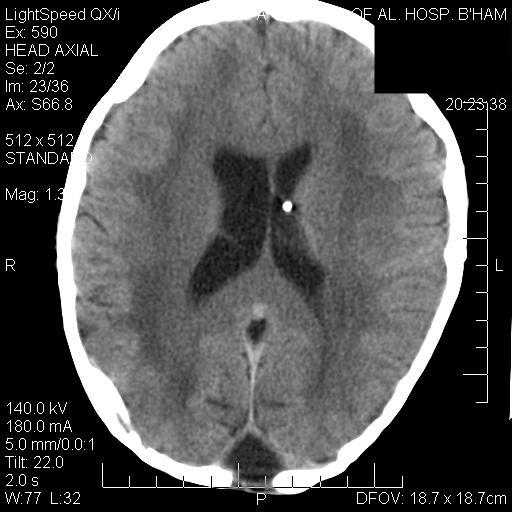
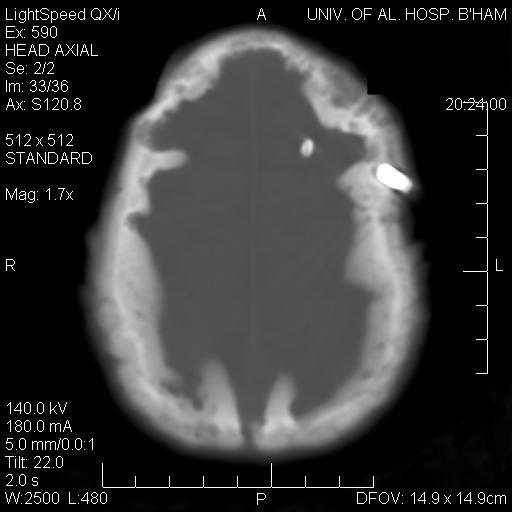
Successful surgical treatment of functional pituitary microadenoma largely relies on accurate identification of the tumor within the sella turcica.These relatively small tumors represent a challenge to both neuroradiologists and neurosurgeons in locating them, resulting in a greater potential for insufficient treatment of the lesion.


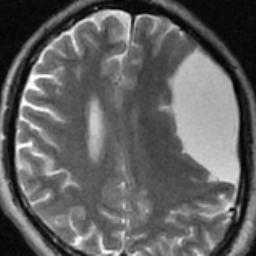
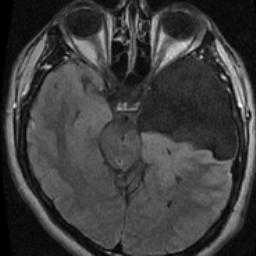
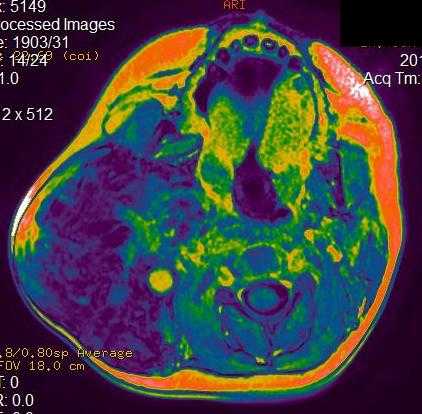
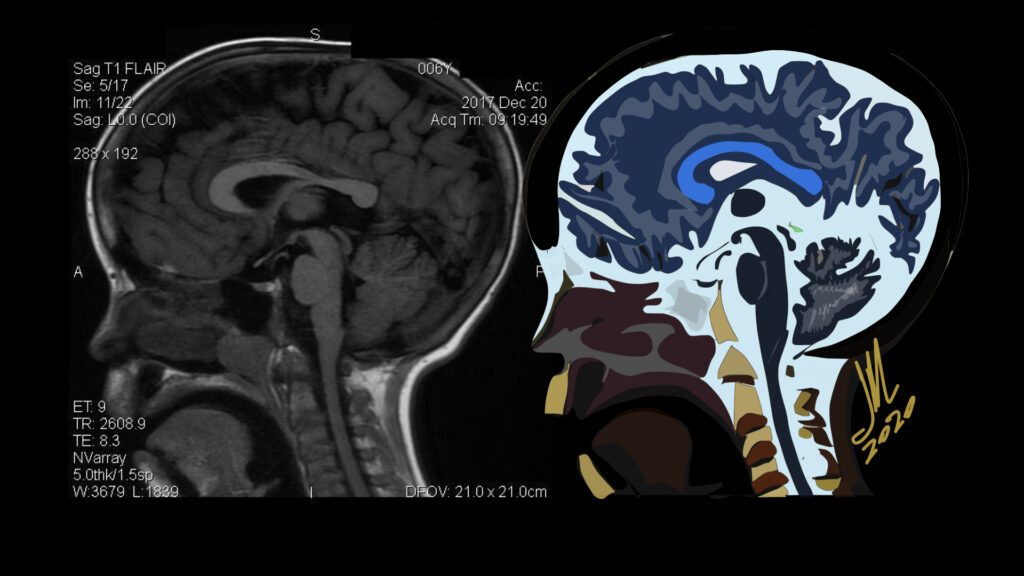
The criterion standard technique used for lesion localization is MR imaging. Dynamic contrast-enhanced technique is often applied on MR imaging to overcome this issue, scanning time usually required to obtain each dynamic phase ranges from 20 to 30 seconds or is shortened into 12–20 seconds in some cases, but it is not possible to obtain a gapless 3D image. The most suitable time phase to obtain sufficient contrast between an adenoma and the normal pituitary gland is 45–60 seconds after contrast agent injection. This adenoma-normal pituitary gland contrast will rapidly diminish within the subsequent 30 seconds. Both spatial and temporal resolution must, therefore, be sufficiently high to visualize the presence of the adenoma.
Acromegaly results from excessive production of growth hormone, most commonly in patients with pituitary adenoma >95% of cases, resulting in the overproduction of insulinlike growth factor 1. Acromegaly is a multisystem disease characterized by somatic overgrowth of osseous structures such as the hands, feet, skull, mandible, and nose. Soft-tissue thickening of the skin and vocal cords and enlargement of internal organs including the heart and kidneys also can be seen. Overproduction of growth hormone before epiphyseal closure leads to linear overgrowth and gigantism